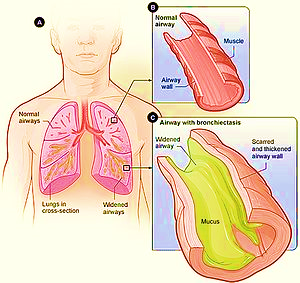
Bronchiectasis is a chronic, irreversible dilation of the bronchi and bronchioles. Under the new definition of COPD, it is considered a disease process separate from COPD (GOLD, 2008).
Bronchiectasis is a condition where the bronchial tubes of your lungs are permanently damaged, widened, and thickened.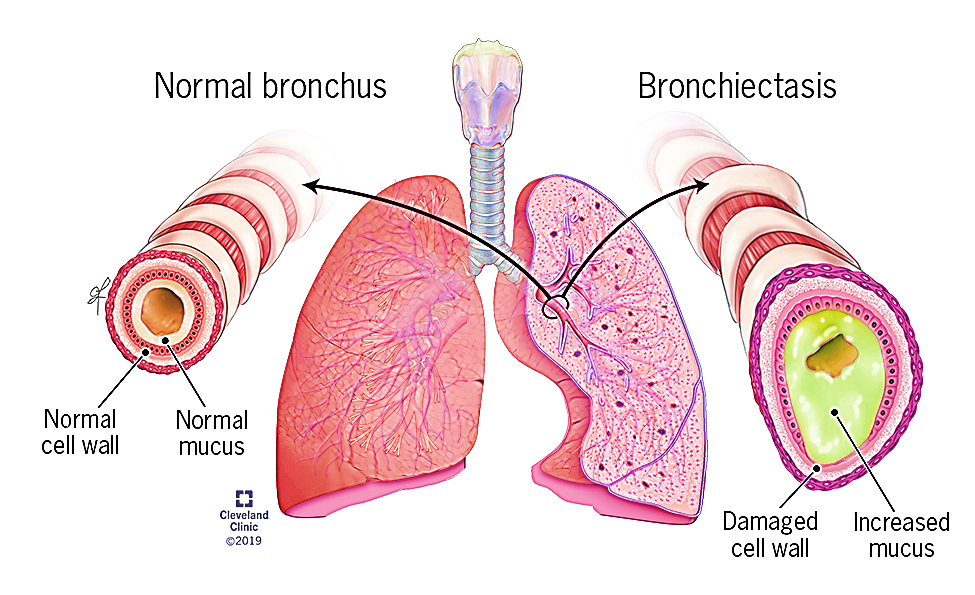
Pathophysiology
Bronchiectasis is an obstructive lung condition in which there is destruction and widening of the large airways and abnormal bronchial wall thickening as a result of a recurring cycle of infection and inflammation (Ten Hacken 2010). Bronchiectasis is usually localised to one lung segment or lobe but may spread over time to other parts of the same lung as a result of unresolved infections. Exacerbations are associated with infections.
A number of conditions lead to bronchiectasis, including structural lung conditions, CF and other conditions associated with abnormal mucocillary clearance; retained inhaled foreign objects, tumours and obstructive lung conditions including COPD; an abnormal immune response; infections including tuberculosis, pneumonia, measles and whooping cough; and inflammatory bowel disease.
Clinical manifestations
- Difficult breathing (dyspnea) due to the mucous production and irritation within the airways.
- Productive, foul-smelling odorous cough, due to thick, difficult-to-expel, tenacious mucous, often with bacterial colonization.
- Cough may be worse when lying down.
- Recurrent bronchial infections.
- Hemoptysis (blood-tinged or bloody mucous).
- Loss of weight because patients are not eating well, due to respiratory changes and foul-smelling mucous with cough. Increased respiratory effort requires more calories to meet normal requirements.
- Crackles or rhonchi on inspiration due to mucous build-up.
- Anemia of chronic disease.
- Cyanosis.
- Clubbing of the fingers.
Causes
Bronchiectasis may be caused by a variety of conditions including:
- Airway obstruction: Obstructions in the bronchi distend the wall permanently and impair mucociliary action.
- Pulmonary infection: Pulmonary infection and obstruction of the bronchus or complications of long-term pulmonary infections cause bronchiectasis.
- Genetic disorders: Genetic disorders such as cystic fibrosis causes the sputum to thicken in consistency and would ultimately obstruct the bronchi.
- Idiopathic causes: There are causes that are unknown to medicine that cause bronchiectasis.
Complications
Potential complications include:
- Atelectasi: Collapse of the alveoli is a common complication.
- Pneumonia: Infection is recurrent in patients with bronchiectasis.
- Empyema: Overproduction of sputum causes the bronchi to be filled with pus.
Diagnosis
- Culture and sensitivity of sputum to identify bacteria and appropriate antibiotics.
- Shadows in affected area of the lungs on the chest x-ray.
- CT scan or high-resolution CT will show areas of bronchiectasis.
- Decreased lung vital capacity on pulmonary function test.
TREATMENT
Treatment is focused on getting enough oxygen to meet current needs of the patient, expel mucous, and treat infections.
- Supplemental oxygen to help meet body’s needs.
- Postural drainage to assist with drainage of secretions.
- Chest PT to loosen secretions.
- Remove excessive secretions during a bronchoscopy.
- Administer bronchodilators to help keep airways open:
- albuterol, levalbuterol
- Administer antibiotics to treat infection:
- selected based on the results of a culture and sensitivity study
NURSING DIAGNOSES
- Ineffective airway clearance
- Imbalanced nutrition: less than what the body requires
- Impaired gas exchange
NURSING INTERVENTION
- Monitor respiratory rate, effort, breath sounds, skin color, and use of accessory muscles.
- Perform chest percussion to help loosen secretions.
- Explain to the patient:
- That family member can perform chest PT.
- How to do postural drainage.
- How to administer oxygen.
- How to properly administer medications.
See videos:
