Key facts
- Hypertension, or high blood pressure, is a life-threatening medical condition that greatly raises the chances of cardiovascular disease, stroke, dementia, and renal failure, and many others.
- It is estimated that 1.28 billion individuals aged 30-79 years worldwide have hypertension, with the majority (two-thirds) living in low- and middle-income countries.
- Additionally, it is estimated that 46 percent of adults with hypertension do not know they have the illness.
- Hypertension is detected in less than half of adult patients (42%).
- Only about a fifth of persons with hypertension (21%) have it under control.
- Premature mortality due to hypertension is a serious global health problem.
What exactly is hypertension?
Blood pressure is the force produced by flowing blood on the arterial walls, the body’s primary blood vessels. Hypertension is too high blood pressure.
Blood pressure is expressed as a pair of numbers. The first number (systolic) shows the blood vessel pressure when the heart contracts or beats. The second number (diastolic) indicates the pressure in the blood arteries between heartbeats.
When tested on two separate days, hypertension is diagnosed if the systolic blood pressure readings on both days are 140 mmHg and/or the diastolic blood pressure readings on both days are 90 mmHg.
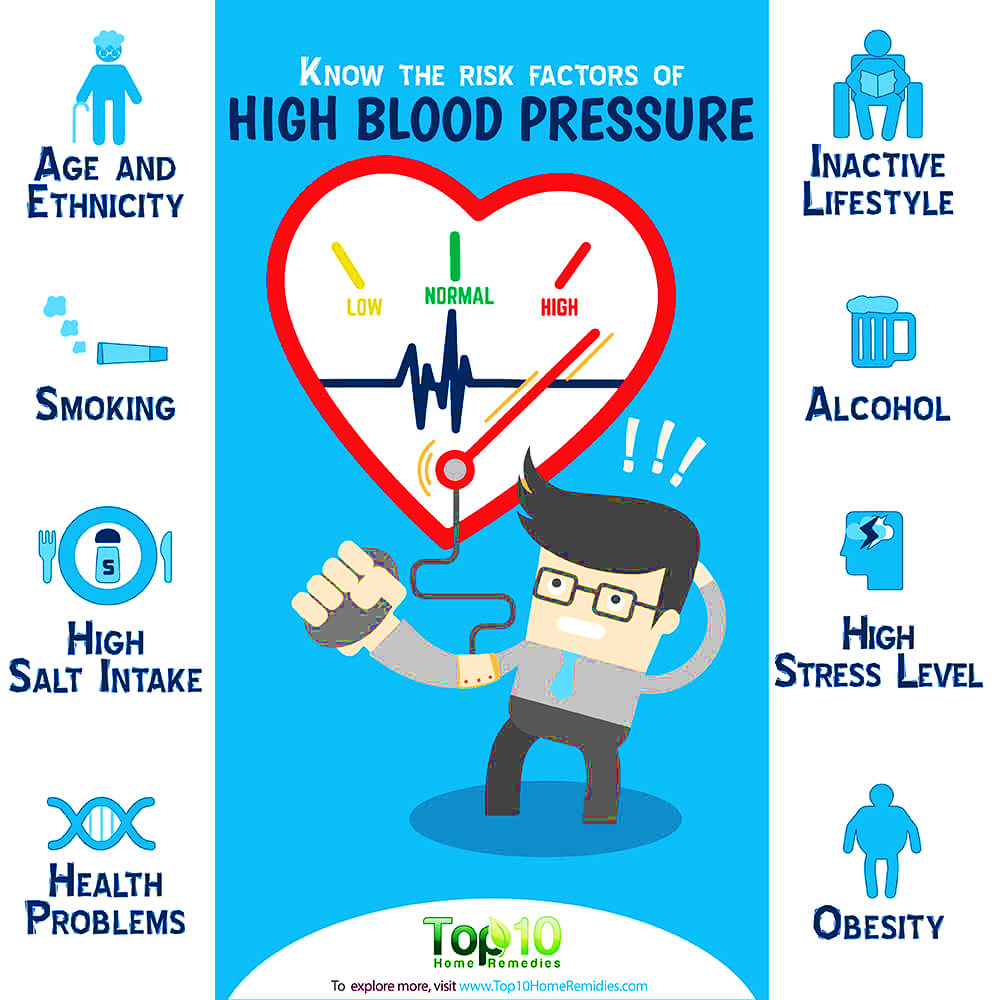
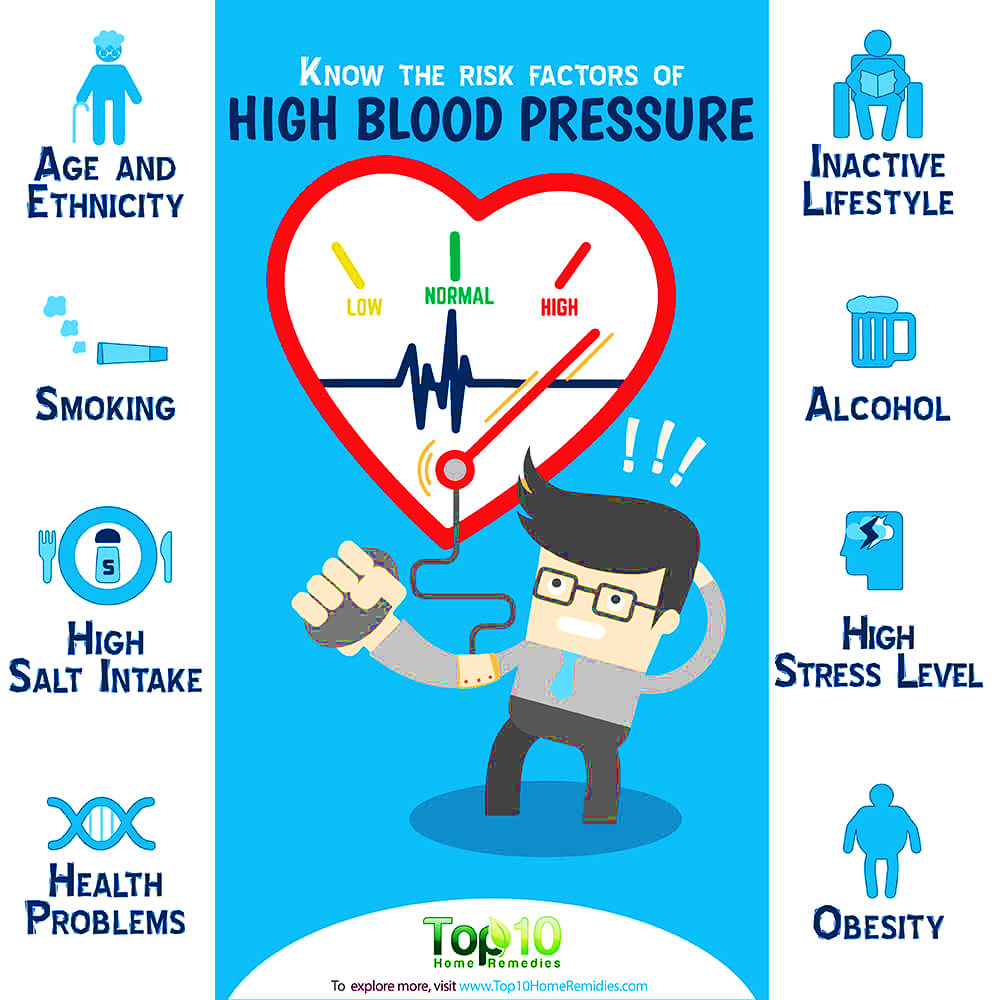 What risk factors are associated with hypertension?
What risk factors are associated with hypertension?
Unhealthy diets (excessive salt consumption, a diet heavy in saturated fat and trans fats, and a poor intake of fruits and vegetables), physical inactivity, cigarette and alcohol use, and being overweight or obese are modifiable risk factors.
Non-modifiable risk factors include a family history of hypertension, age over 65, and coexisting conditions like diabetes or renal illness.
Pathophysiology Of Primary Hypertension
Hypertension is characterised by a consistently elevated SVR.
Retention of water and sodium: A high sodium intake may activate many pressor systems and produce water retention.
High plasma renin activity (PRA) causes an increase in the conversion of angiotensinogen to angiotensin I, which causes arteriolar constriction, vascular hypertrophy, and aldosterone production.
Stress and increased SNS activity: Anger, fear, and pain have an effect on arterial pressure. Normally protective physiological reactions to stress may continue to a pathologic degree, resulting in a protracted increase in SNS activity. Enhanced SNS activation results in increased vasoconstriction, heart rate, and renin release.
Insulin resistance and hyperinsulinemia are frequent in primary hypertension, as are abnormalities of glucose, insulin, and lipoprotein metabolism. Vascular hypertrophy and enhanced renal salt reabsorption are supplementary pressor effects of insulin.
Endothelial cell dysfunction is characterised by a diminished vasodilator response to nitric oxide in some hypertensive individuals. Nitric oxide, an endothelium-derived relaxing factor (EDRF), helps maintain low arterial tone at rest, inhibits smooth muscle layer development, and prevents platelet aggregation. Vasoconstriction produced by endothelin is pronounced and protracted.
 What are common hypertension symptoms?
What are common hypertension symptoms?
Hypertension is referred to as the “silent killer.” The majority of hypertensive individuals are unaware of their condition, since there may be no warning indications or symptoms. Therefore, it is crucial that blood pressure be monitored often.
When symptoms do manifest, they might include headaches in the early morning, nosebleeds, abnormal heart rhythms, visual problems, and a buzzing sound in the ears. Severe hypertension may result in tiredness, nausea, vomiting, disorientation, anxiety, chest discomfort, and tremors.
A professional measurement of blood pressure is the sole method for detecting hypertension. The measurement of blood pressure is rapid and painless. Individuals may test their own blood pressure using automated equipment, but a professional examination is necessary for assessing risk and related problems.
What are the complications of hypertension that is uncontrolled?
In addition to other issues, hypertension may cause severe heart damage. Excessive pressure may cause artery hardening, reducing blood and oxygen flow to the heart. This increased blood pressure and decreased blood flow may result in:
- Chest discomfort, often known as angina.
- Heart attack, which happens when the heart’s blood flow is obstructed and heart muscle cells are deprived of oxygen, is fatal. The longer the heart is deprived of blood flow, the worse the cardiac damage.
- Heart failure occurs when the heart is unable to pump sufficient blood and oxygen to other critical organs.
The irregular heartbeat that might cause abrupt death.
Additionally, hypertension may rupture or obstruct the arteries that feed blood and oxygen to the brain, resulting in a stroke.
Additionally, hypertension may damage the kidneys, leading to renal failure.
Why is hypertension a significant problem in low- and middle-income nations?
The prevalence of hypertension varies by geography and socioeconomic level within a nation. The WHO African Region has the greatest prevalence of hypertension at 27%, whilst the WHO American Region has the lowest incidence at 18%.
From 1975 to 2015, the number of individuals with hypertension grew from 594 million to 1.13 billion, with the majority of the rise occurring in low- and middle-income nations. This increase is mostly attributable to an increase in hypertension risk factors in these groups.
How may the consequences of hypertension be reduced?
Reducing hypertension avoids heart attacks, strokes, and renal damage, among other health complications.
Prevention
- reducing salt consumption (to less than 5g daily).
- Increasing consumption of fruits and vegetables.
- Physical activity on a regular basis.
- avoiding tobacco usage.
- reducing the amount of alcohol consumed.
- Restricting consumption of foods rich in saturated fats.
- Dietary elimination or reduction of trans fats.
Management
- Stress reduction and management.
- Routinely monitoring blood pressure.
- The treatment of high blood pressure
- Managing additional health issues.
Nursing Management
Primary nursing duties for the long-term management of hypertension include assisting the patient in lowering blood pressure and adhering to the treatment plan. The nursing interventions include patient and family education, detection and reporting of adverse treatment effects, assessment and improvement of compliance, and evaluation of therapeutic efficacy.
Patient and family-centered instruction involves the following:
(1) dietary treatment,
(2) pharmacological therapy,
(3) physical exercise,
(4) home monitoring of blood pressure (if appropriate), and
(5) cessation of cigarette use (if applicable).

 What risk factors are associated with hypertension?
What risk factors are associated with hypertension? What are common hypertension symptoms?
What are common hypertension symptoms?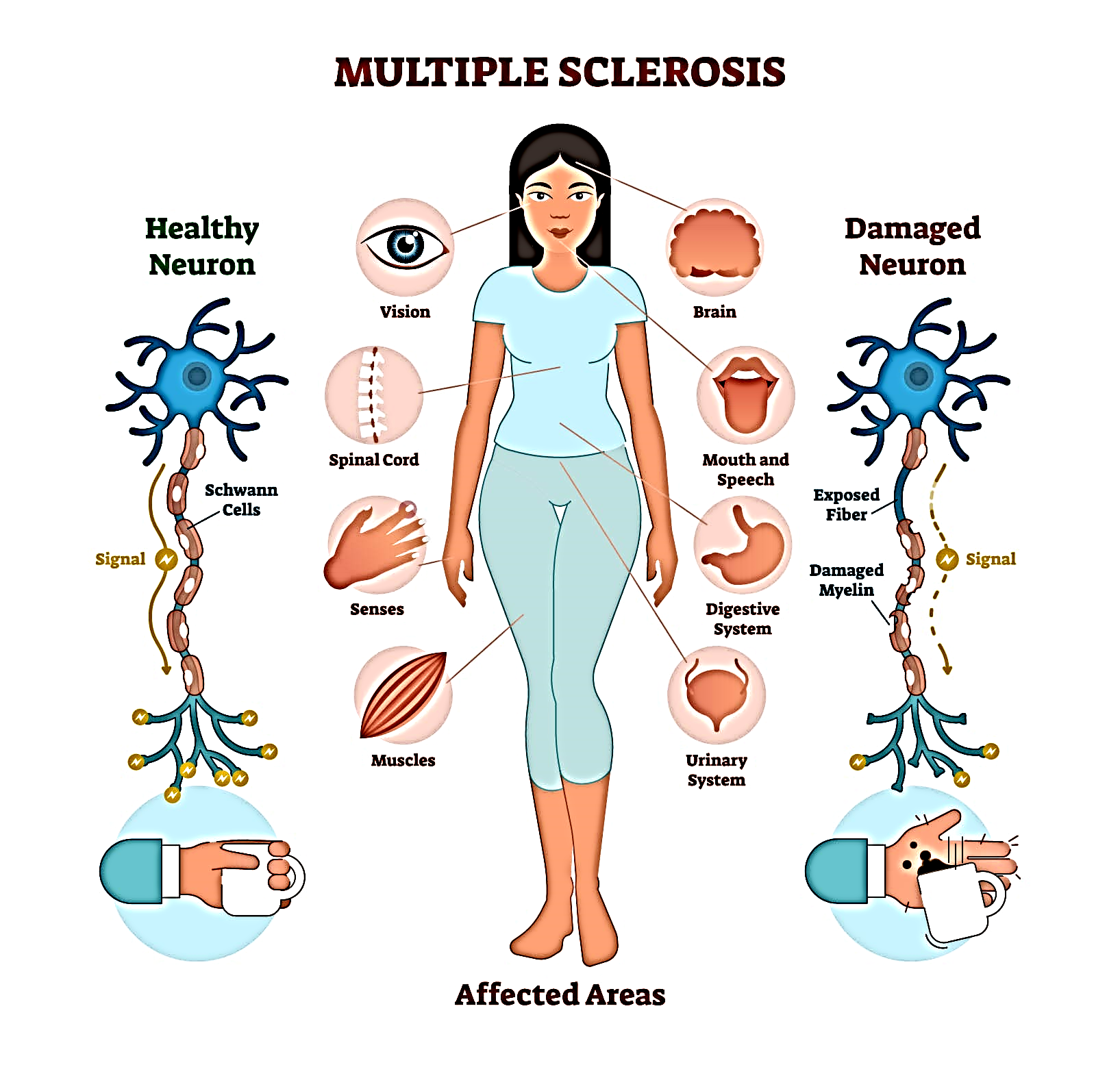 Multiple sclerosis is a disease that causes vision problems, numbness and tingling, muscle weakness, and other problems. It happens when the body’s infection-fighting system attacks and damages nerve cells and their connections in the brain and spinal cord. When the body’s infection-fighting system, called the “immune system,” attacks the body’s own cells, it is called an “autoimmune response.” It causes damage to myelin, the protective coating around the nerves. When myelin is damaged, messages can no longer be clearly transmitted from the brain and spinal cord to other parts of the body. Many people refer to multiple sclerosis as “MS.” INCIDENCE
Multiple sclerosis is a disease that causes vision problems, numbness and tingling, muscle weakness, and other problems. It happens when the body’s infection-fighting system attacks and damages nerve cells and their connections in the brain and spinal cord. When the body’s infection-fighting system, called the “immune system,” attacks the body’s own cells, it is called an “autoimmune response.” It causes damage to myelin, the protective coating around the nerves. When myelin is damaged, messages can no longer be clearly transmitted from the brain and spinal cord to other parts of the body. Many people refer to multiple sclerosis as “MS.” INCIDENCE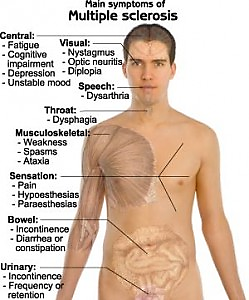 the most debilitating factor, even for those who have minimal physical restrictions, and is one of the leading causes for people leaving the workforce.
the most debilitating factor, even for those who have minimal physical restrictions, and is one of the leading causes for people leaving the workforce.