Tuberculosis affects primarily the lungs and gastrointestinal tract, but may also infect the musculoskeletal system.
Pathology
- Hematogenous dissemination to long bones and vertebrae
- Direct spread to bone from adjacent tuberculous lymphadenitis
- Single or multi centric, particularly in AIDS
- Predilection for synovium – higher oxygen pressure
There is caseating granulomatous inflammation with bone necrosis, resulting in the destruction of bone.
Extension of the TB osteomyelitis into joint spaces results in tuberculous arthritis. The infection crosses to the bone on the other side of the joint.
Incidence
- 3% of tuberculosis is musculoskeletal. Of these, the commonest area affected is the spine.
Radiological signs
- Lytic process.
- Affects both sides of a joint or disc space.
- Soft tissue swelling
- Effusion in a joint
- Paravertebral swelling in thorax
- Fusiform paravertebral swelling in the neck
- Cystic tuberculosis – causes cystic lesions in bones
Sclerosis is a sign of healing TB – successfully treated lesions become sclerotic as they heal.
Special Investigations
The ESR is raised often to above 100 mm/hr. On the differential white cell count there is a lymphocytosis. Sputum is taken for culture and a 24 hour urine collection can be taken if renal tuberculosis is a suspected cause.
Serological tests such as the Mantoux or Tine test are positive. In a third world population, such as South Africa there is anyway a high incidence of positivity with these tests. A positive test merely indicates that a patient has had exposure to TB in the past. A negative test may be of more value in excluding TB, but other immunosuppressive diseases such as HIV may suppress the reaction.
Biopsy
Biopsy may be needed is the diagnosis is in doubt. In South Africa, where tuberculosis is common, biopsy is not always done. If the blood and radiological criteria point to Tuberculosis therapy is started without a biopsy
Treatment
Anti tuberculous drugs are started.
(South African Medicines Formulary, fifth edition pg. 277)
Antituberculosis Drugs for Adults
| Intensive phase (2 –3 months): | Body weight <50kg | >50kg |
| Rifampisin 120mg +Isoniasid (INH) 60 mg + Pirasinamide (PZA) 300mg + Etambutol 200mgCombination tablet (Rifafour®, Myrin Plus®) daily, 5 days per week | 4 tablets daily | 5 tablets daily |
| Maintenance phase: | <50kg | >50kg |
| Rifampisin 150mg + INH 100mgRifampisin 300mg + INH 150mg | 3 tablets daily- | -2 tablets daily |
Pyridoxine (Vitamin B6) 10mg /day must be added in patients with inadequate intake, or at risk of developing peripheral neuropathy (pregnancy, diabetics, HIV infected patients)
Therapy lasts at least 1 year to 18 months. The ESR should show a decrease and the lesion on X rays becomes more sclerotic.
Failure to respond may be due to:-
- Failure to take the drugs
- Wrong diagnosis
- Drug resistant tuberculosis
Side effects of anti tuberculous drugs
| Serious: | Drug causing | Action |
| Jaundice (hepatitis) | INH, Rifampisin, PZA | Stop TB Drugs. Contact an infection specialist. |
| Skin rash with pyrexia | INH, Rifampisin | |
| Bleeding tenancy, shock, renal failure. | Rifampisin | |
| Impaired vision and color perception | Etambutol |
Splinting of joints
The affected joint must be immobiliased in a position of function. For the hip in the acute phase it means skin traction. Once discharged from hospital the patient with hip TB is told to sleep prone to avoid a flexion contracture. The spine will need an appropriate brace. For other joints a plaster cast, back slab or a custom made splint may be necessary
Place of Surgery
Surgery plays a limited role in the treatment of tuberculosis. Synovial biopsy may be needed to make the diagnosis. In spinal tuberculosis, gross instability or neurological fallout are indications for an anterior fusion and decompression.
Late surgery may be needed to repair the damage by a joint being destroyed or left in an unacceptable position. Arthrodesis is sometimes the only solution in these severe cases.
Spinal Tuberculosis
In the thoracic spine the patient presents with a gibbus.
There may be neurological fallout due to:
- Mechanical pressure on the spinal cord
- Vascular – blood supply to cord compromised
- TB granuloma pressing on cord
Radiology
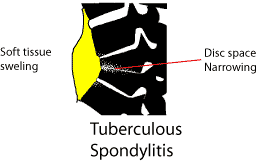
There is loss of disc space, soft tissue swelling is commonly seen adjacent to the involved area, or the pus may track into the psoas sheath (involvement about thoraco-lumbar junction)
Treatment principles remain the same as with TB of other areas. Antituberculosis medication is begun once the diagnosis is confirmed. Further deformity is prevented with a hard brace such as a Thoraco sacro lumbar orthosis (for Thoraco-lumbar involvement).
An indication for operation is neurological compromise, unresponsive to treatment. As TB spine involves mainly the vertebral body, an anterior approach is needed. The caseous material is curetted out and the vertebral bodies fused with an anterior bone graft. The rib removed for the thoracotomy can be used for this.
