1. What is the meaning of morbidity?
a) Health
b) Treatment
c) Care
d) Illness.
2. _____________is the number of deaths during the first year of life per 1000 live births?
a) Neonatal morbidity rate
b) Birth rate
c) Illness rate
d) Infant mortality rate.
3. What are the Factors affecting on infant mortality rate except?
a) Birth weight
b) Low level of maternal education
c) Full term birth.
d) Male gender
4. The MOST common cause of under-5 mortality in developing world is
a) Neonatal disease.
b) Diarrhea
c) Malaria
d) Measles
5. After the first year of life, the MOST common cause of death in children is mainly
a) Drowning
b) Burn
c) Accident.
d) War
6. The MOST successful injury prevention strategy is
a) Car seats
b) Water safety
c) Poison prevention.
d) Fall prevention
7. Regarding the physical growth of preschool children (3-5 yr); all the following are true EXCEPT
a) 4-5 kg weight increment/yr.
b) 6-7 cm height increment/yr
c) Brain myelinization stops by 8 yr
d) First deciduous tooth falls by 6 yr
8. Regarding the physical growth of middle childhood (6-11 yr); all the following are true EXCEPT
a) 3-3.5 kg wt increment/yr
b) 6-7 cm height increment/yr
c) Brain myelinization stops by 8 yr.
d) First deciduous tooth falls by 6 yr
9. In fetal period, all the following are true EXCEPT
a) 10 weeks the midgut returns to abdomen
b) 24 weeks surfactant production begun
c) 26 weeks recognizable human face formed.
d) During third trimester the weight triples
10. Prenatal exposure to cigarette smoke is associated with
a) Lower birthweight
b) Shorter length
c) Neonatal diabetes.
d) Learner problem
11. The age at which the infant achieve early head control with bobbing motion when pulled to sit is
a) 2 months
b) 3 months.
c) 3 months
d) 4 months
12. The age at which the infant can reach an object, grasp it and bring it to mouth and seems exited when see the food is
a) 4 months.
b) 5 months
c) 6 Month
d) 7 Month
13. By the age of 7 months the infant is able to do all the following EXCEPT
a) Transfer object from hand to hand
b) Bounces actively
c) Grasp uses radial palm
d) Cruises.
14. A 10-month-old child can do all the following EXCEPT
a) Says “mama” or “dada”
b) Points to objects
c) Speaks first real word.
d) Follows one-step command without gesture
15. The first permanent tooth to erupt is
a) Central incisor at 6 yr
b) Molar at 6 yr.
c) Premolar at 6-7 yr
d) Upper canine at 6-7 yr
16. The MOST common cause of sleeping difficulty in the first 2 months of life is
a) Gastro-esophageal reflux
b) Formula intolerance
c) Colic
d) Developmentally sleeping behavior.
17. All the following are compatible with the definition of obstructive sleep apnea EXCEPT
a) Repeated episodes of prolonged upper airway obstruction
b) ≥30% reduction in airflow
c) Apnea
d) ≥ 30% O2 desaturation.
18. following, the MOST common cause of obstructive sleep apnea in children is
a) Adenotonsillar hypertrophy.
b) Allergy
c) Obesity
d) Craniofacial abnormalities
19. Persons with Down syndrome are at particularly high risk for obstructive sleep apnea with up to 70% prevalence. All the following are considered as risk factors EXCEPT
a) Peculiar facial anatomy
b) Hypotonia
c) Developmental delay.
d) Hypothyroidism
20. All the following are parasomnia disorders EXCEPT
a) Narcolepsy.
b) Sleepwalking
c) Confusional arousal
d) Nightmare
21. The neurodevelopmental function (cognition) is dependent mainly on the development of the following functions EXCEPT
a) Visual–spatial
b) Sensory & Motor
c) Cerebellar.
d) Language
22. The major chemical modulator of attention is
a) Troponin
b) Serotonin
c) Dopamine.
d) Epinephrine
23. All the following are risk factors for specific learning disorders (SLD) EXCEPT
a) Extreme prematurity
b) Low birth weight
c) History of admission to neonatal care unit.
d) History of sibs or parents with SLD
24. All the following are red flags in the history of children with specific learning disorders (SLD) EXCEPT
a) Inconsistency in marks report from grade to grade.
b) Struggling with homework activities
c) Struggling with homework activities
d) Positive standard screening test
25. All the following are established modalities of treatment in a child with specific learning disorders (SLD) EXCEPT
a) remediation of skills
b) demystification
c) bypass strategies
d) Dietary interventions.
26. The MOST common specific learning disorder (SLD) of childhood is
a) attention-deficit/hyperactivity disorder (ADHD)
b) Reading disorder (dyslexia).
c) spelling disorder
d) arithmetical skills disorders
27. You are assessing an eight-year-old male child with attention-deficit/hyperactivity disorder (ADHD). Following, the LEAST useful test/investigation is
a) thyroid function test
b) EEG
c) Blood film.
d) Polysomnography
28. Following of the MOST common presenting behavior in girls with attention deficit/ hyperactivity disorder (ADHD) is
a) Inattentive.
b) Hyperactive
c) Impulsive
d) Disruptive
29. Which of the following is TRUE statement of reading disorder?
a) 25% of affected children have affected parents
b) Diagnosis is usually clinical.
c) IQ will remain same with time
d) boys are more affected than girls
30. The MOST reported type of child abuse in Pakistan is
a) Neglect
b) Sexual abuse.
c) Physical abuse
d) psychological maltreatment
Category Archives: Pediatrics Nursing
Dengue fever
 Dengue fever is a mosquito-borne viral infection that can cause flu-like symptoms and, in severe cases, potentially life-threatening complications. It is caused by the dengue virus, which is transmitted to humans primarily through the bite of infected female Aedes mosquitoes, particularly Aedes aegypti and Aedes albopictus. Dengue fever is common in tropical and subtropical regions of the world, including parts of Southeast Asia, the Pacific Islands, the Caribbean, and Central and South America.
Dengue fever is a mosquito-borne viral infection that can cause flu-like symptoms and, in severe cases, potentially life-threatening complications. It is caused by the dengue virus, which is transmitted to humans primarily through the bite of infected female Aedes mosquitoes, particularly Aedes aegypti and Aedes albopictus. Dengue fever is common in tropical and subtropical regions of the world, including parts of Southeast Asia, the Pacific Islands, the Caribbean, and Central and South America.
Here are some key points about dengue fever:
Symptoms:
The symptoms of dengue fever typically appear 4-10 days after being bitten by an infected mosquito and can include high fever, severe headache, pain behind the eyes, joint and muscle pain, rash, and mild bleeding. In some cases, dengue fever can progress to a more severe form known as dengue hemorrhagic fever or dengue shock syndrome, which can be life-threatening.
Dengue fever presents with a wide range of signs and symptoms that can vary in severity. The disease typically has an incubation period of 4-10 days after being bitten by an infected mosquito. The symptoms of dengue fever can be categorized into three phases: the febrile phase, the critical phase, and the recovery phase. Not all individuals with dengue infection will progress through all three phases, and the severity of symptoms can vary from mild to severe. Here are the common signs and symptoms associated with each phase:
- Febrile Phase (Acute Phase):
High Fever: Sudden onset of high fever, often reaching up to 104°F (40°C).
Severe Headache: Intense frontal headache, which is a common feature of dengue fever.
Pain Behind the Eyes: Pain or discomfort, especially when moving the eyes.
Joint and Muscle Pain: Severe joint and muscle pain, often referred to as “breakbone fever.”
Rash: A rash may develop, typically starting a few days after the onset of fever. It can be maculopapular (red and raised) and sometimes itchy.
Fatigue: Extreme fatigue and weakness.
Nausea and Vomiting: Some individuals may experience nausea and vomiting.
Mild Bleeding: Minor bleeding manifestations such as nosebleeds, gum bleeding, or easy bruising can occur.
- Critical Phase (Warning Signs):
Around the 3-7 day mark, some patients with dengue fever may progress to a critical phase. Warning signs indicate increased severity and the potential for complications. These signs include:
Persistent Abdominal Pain: Severe abdominal pain may develop, which can be a sign of impending complications like dengue hemorrhagic fever.
Vomiting with Blood: Vomiting blood (hematemesis) or passing blood in the stool (melena) can occur.
Bleeding: Severe bleeding, such as from the nose or gums, petechiae (small red or purple spots on the skin), or hematuria (blood in the urine).
Rapid Breathing: Increased respiratory rate and difficulty breathing.
Cold or Clammy Skin: Skin may become cold, pale, or clammy.
Restlessness: Agitation or restlessness may be observed.
- Recovery Phase:
After the critical phase, most patients gradually recover over the next few days to weeks.
The fever subsides, and other symptoms begin to improve.
Convalescence: Patients may experience fatigue and weakness during the recovery phase, which can persist for an extended period.
It’s important to note that not all individuals with dengue fever progress to the critical phase or develop severe symptoms. The majority of cases are mild, and with proper medical care and supportive treatment, the prognosis is usually favorable. However, severe dengue (such as dengue hemorrhagic fever or dengue shock syndrome) can be life-threatening and requires immediate medical attention.
If you or someone you know exhibits the warning signs of dengue fever, it’s crucial to seek medical care promptly to prevent complications and ensure appropriate treatment and monitoring.
Diagnosis: Dengue fever is usually diagnosed through blood tests that detect the presence of the dengue virus or antibodies produced in response to the virus.
Laboratory findings play a significant role in the diagnosis and management of dengue fever. The results of various laboratory tests can help confirm the presence of the dengue virus, assess the severity of the infection, and guide treatment decisions. Here are some of the key laboratory findings associated with dengue fever:
Dengue Serology (Antibody Tests):
IgM Antibodies: In the early stages of the illness (usually within the first week), dengue-specific IgM antibodies can be detected in the patient’s blood. The presence of IgM antibodies suggests a recent dengue infection.
IgG Antibodies: Dengue-specific IgG antibodies may appear later and persist for a more extended period. Elevated IgG levels may indicate a past dengue infection.
Polymerase Chain Reaction (PCR) Test:
Dengue PCR: This test detects the genetic material (RNA) of the dengue virus in a patient’s blood. It is most useful in the early days of infection, even before the appearance of IgM antibodies. PCR can help confirm an acute dengue infection and identify the specific serotype of the virus.
Complete Blood Count (CBC):
Platelet Count: One of the hallmark laboratory findings in dengue fever is a decrease in platelet count (thrombocytopenia). Platelets are essential for blood clotting, and low platelet levels can lead to bleeding tendencies.
Hematocrit (Hct) Levels: An elevated hematocrit (a measure of the proportion of red blood cells in the blood) can indicate hemoconcentration, which is common in dengue fever due to plasma leakage.
Liver Function Tests:
AST (Aspartate Aminotransferase) and ALT (Alanine Aminotransferase): Elevated levels of these liver enzymes are often seen in dengue patients, indicating liver involvement.
Coagulation Profile:
PT (Prothrombin Time) and APTT (Activated Partial Thromboplastin Time): These tests assess the blood’s clotting ability. Prolonged PT and APTT may be seen in severe cases of dengue with bleeding tendencies.
Electrolyte Levels:
Sodium (Na) and Potassium (K): Abnormal electrolyte levels can occur due to fluid imbalances in dengue patients, especially those with severe symptoms.
Creatinine and Urea Levels:
Kidney Function Tests: Elevated creatinine and urea levels may indicate kidney involvement in severe dengue cases.
Other Tests:
NS1 Antigen Test: This test can detect the presence of the dengue virus NS1 antigen in a patient’s blood and is useful for early diagnosis.
Dengue Serotyping: In areas with multiple dengue virus serotypes, it’s important to identify the specific serotype causing the infection as some serotypes are associated with more severe disease.
Laboratory findings in dengue fever can vary depending on the stage of the infection and the severity of the disease. These tests help healthcare providers confirm the diagnosis, assess the patient’s condition, and make decisions regarding treatment and monitoring. It’s important to note that dengue fever is a dynamic disease, and laboratory findings may change over the course of the illness, so repeated testing and close monitoring are often necessary, especially in severe cases.
Prevention:
The best way to prevent dengue fever is to avoid mosquito bites. This can be achieved by using insect repellent, wearing long-sleeved clothing, and staying in air-conditioned or screened-in accommodations. Additionally, efforts to reduce mosquito breeding sites, such as eliminating standing water around homes, are essential for dengue prevention.
Vaccination:
As of my last knowledge update in September 2021, there was an approved dengue vaccine called Dengvaxia. However, its use and availability varied by country, and it was primarily recommended for individuals who had previously been infected with dengue. Vaccine availability and recommendations may have evolved since then, so it’s essential to check with local health authorities for the most up-to-date information on dengue vaccines.
It’s important to note that dengue fever can be a serious illness, and early detection and medical care are crucial for managing the disease effectively, especially in severe cases. If you suspect you have dengue fever or are in an area where the disease is prevalent, seek medical attention promptly.
Treatment:
There is no specific antiviral treatment for dengue fever. Management primarily involves relieving the symptoms and providing supportive care, such as staying hydrated and taking pain relievers like acetaminophen. Aspirin and non-steroidal anti-inflammatory drugs (NSAIDs) should be avoided because they can increase the risk of bleeding.
The medical and nursing management of dengue fever involves a combination of supportive care and monitoring to alleviate symptoms, prevent complications, and promote recovery. Here’s a comprehensive overview of the medical and nursing management of dengue fever:
Medical Management:
Diagnosis: Accurate diagnosis through clinical evaluation and laboratory tests (serology or PCR) is essential to confirm dengue fever.
Hospitalization: Depending on the severity of the illness, some patients may require hospitalization. Hospitalization is especially crucial for patients with severe dengue or those at risk of complications.
Fluid Replacement: Adequate hydration is a cornerstone of dengue management. Intravenous (IV) fluids are often administered to maintain fluid and electrolyte balance. Nurses closely monitor patients’ fluid intake and output.
Pain and Fever Management: Analgesics such as acetaminophen are given to relieve pain and reduce fever. Non-steroidal anti-inflammatory drugs (NSAIDs) and aspirin should be avoided, as they can increase the risk of bleeding.
Monitoring: Regular monitoring of vital signs, hematocrit levels, platelet counts, and other relevant parameters is crucial to assess the progression of the disease and the patient’s response to treatment.
Blood Transfusion: In severe cases of dengue with hemorrhagic manifestations, blood transfusion may be necessary to replace lost blood components.
Nursing Management:
Assessment: Nurses conduct a thorough assessment of the patient’s clinical status, including vital signs, hydration level, skin condition, and the presence of bleeding or shock symptoms.
Fluid Administration: Nurses administer IV fluids as prescribed by the physician, ensuring that the rate and type of fluid are appropriate for the patient’s condition.
Monitoring: Frequent monitoring of vital signs, especially blood pressure, pulse rate, and respiratory rate, is essential to detect any deterioration in the patient’s condition promptly.
Pain and Fever Control: Nurses administer pain relievers and antipyretics as ordered by the physician and monitor the patient’s response to these medications.
Emotional Support: Providing emotional support and reassurance to the patient and their family is essential, as dengue fever can be a distressing experience.
Education: Nurses educate patients and their families about the importance of hydration, medication compliance, and the signs and symptoms that require immediate medical attention.
Infection Control: Nurses ensure strict infection control measures to prevent the spread of the virus, particularly in healthcare settings. This includes proper hand hygiene and personal protective equipment (PPE) use.
Patient Education: Patients should be educated about the prevention of mosquito bites and the importance of seeking prompt medical care if their condition worsens.
Discharge Planning: When the patient is stable and ready for discharge, nurses provide instructions for continued care at home, including medication schedules and follow-up appointments.
The medical and nursing management of dengue fever should be tailored to the individual patient’s condition and may vary based on the severity of the illness. Close collaboration between healthcare providers, including physicians, nurses, and other healthcare staff, is crucial to ensure optimal patient care and recovery.
Cystic Fibrosis
Cystic fibrosis (CF) is the most common fatal autosomal recessive disease among the Caucasian population. An individual must inherit a defective copy of the CF gene (one from each parent) to have CF. Cystic fibrosis is usually diagnosed in infancy or early childhood, but patients may be diagnosed later in life. For individuals diagnosed later in life, respiratory symptoms are frequently the major manifestation of the disease.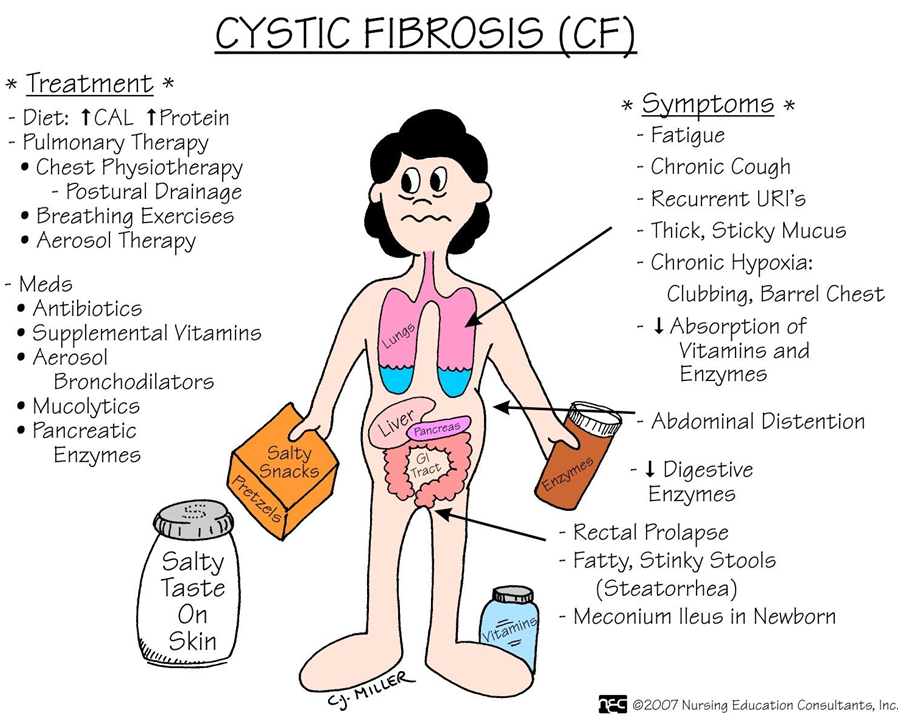
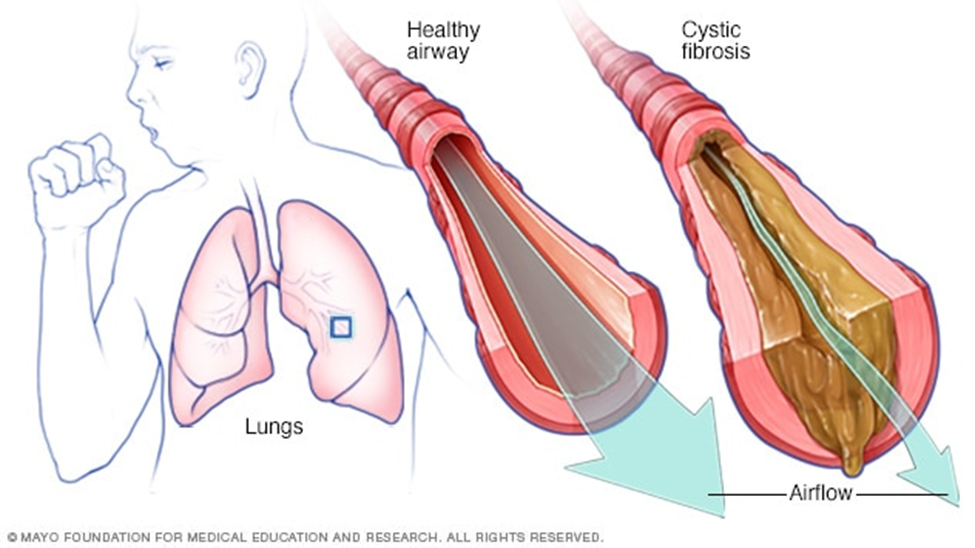
Pathophysiology
This disease is caused by mutations in the CF transmembrane conductance regulator protein, which is a chloride channel found in all exocrine tissues. Chloride transport problems lead to thick, viscous secretions in the lungs, pancreas, liver, intestine, and reproductive tract as well as increased salt content in sweat gland secretions. In 1989, major breakthroughs were made in this disease with the identification of the CF gene. The ability to detect the common mutations of this gene allows for routine screening for this disease as well as the detection of carriers. Genetic counseling is an important part of health care for couples at risk.
Airflow obstruction is a key feature in the presentation of CF. This obstruction is due to bronchial plugging by purulent secretions, bronchial wall thickening due to inflammation, and, over time, airway destruction. These chronic retained secretions in the airways set up an excellent reservoir for continued bronchial infections.
Clinical Manifestations
The pulmonary manifestations of this disease include;
- a productive cough, wheezing, hyperinflation of the lung fields on chest x-ray, and pulmonary function test results consistent with obstructive airways disease.
- Colonization of the airways with pathogenic bacteria usually occurs early in life.
- Staphylococcus aureus and Haemophilus influenzae are common organisms during early childhood. As the disease progresses, Pseudomonas aeruginosa is ultimately isolated from the sputum of most patients.
- Upper respiratory manifestations of the disease include sinusitis and nasal polyps.
Nonpulmonary clinical manifestations include;
- gastrointestinal problems (eg, pancreatic insufficiency, recurrent abdominal pain, biliary cirrhosis, vitamin deficiencies, recurrent pancreatitis, weight loss),
- genitourinary problems (male and female infertility), and
- Clubbing of the extremities.
Assessment and Diagnostic Findings
Most of the time, the diagnosis of CF is made based on an elevated result of a sweat chloride concentration test, along with clinical signs and symptoms consistent with the disease. Repeated sweat chloride values of greater than 60 mEq/L distinguish most individuals with CF from those with other obstructive diseases. A molecular diagnosis may also be used in evaluating common genetic mutations of the CF gene.
Medical Management
Pulmonary problems remain the leading cause of morbidity and mortality in CF. Because chronic bacterial infection of the airways occurs in individuals with CF, control of infections is key in the treatment.
- Antibiotic medications are routinely prescribed for acute pulmonary exacerbations of the disease. Depending upon the severity of the exacerbation, aerosolized, oral, or intravenous antibiotic therapy may be used. Antibiotic agents are selected based upon the results of a sputum culture and sensitivity. Patients with CF have problems with bacteria that are resistant to multiple drugs and require multiple courses of antibiotic agents over long periods of time.
- Bronchodilators are frequently administered to decrease airway obstruction. Differing pulmonary techniques are used to enhance secretion clearance. Examples include manual postural drainage and chest physical therapy, high-frequency chest wall oscillation, and other devices that assist in airway clearance (PEP masks [masks that generate positive expiratory pressure], “flutter devices” [devices that provide an oscillatory expiratory pressure pattern with positive expiratory pressure and assist with expectoration of secretions]).
- Inhaled mucolytic agents such as dornase alfa (Pulmozyme) or N-acetylcysteine (Mucomyst) may also be used. These agents help to decrease the viscosity of the sputum and promote expectoration of secretions.
- Anti-inflammatory: To decrease the inflammation and ongoing destruction of the airways, anti-inflammatory agents may also be used. These may include inhaled corticosteroids or systemic therapy. Other anti-inflammatory medications have also been studied in CF. Ibuprofen was studied in children with CF and some benefit was demonstrated, but there is little information on its use in young or older adults with CF.
- Supplemental oxygen is used to treat the progressive hypoxemia that occurs with CF. It helps to correct the hypoxemia and may minimize the complications seen with chronic hypoxemia (pulmonary hypertension).
- Lung transplantation is an option for a small, select population of CF patients. A double lung transplant technique is used due to the chronically infected state of the lungs seen in end-stage CF. Because there is a long waiting list for lung transplant recipients, many patients die while awaiting a transplant.
- Gene therapy is a promising approach to management, with many clinical trials underway. It is hoped that various methods of administering gene therapy will carry healthy genes to the damaged cells and correct defective CF cells. Efforts are underway to develop innovative methods of delivering therapy to the CF cells of the airways.
Nursing Diagnosis
Based on the assessment data, the major nursing diagnoses are:
- Ineffective airway clearance related to thick, tenacious mucus production.
- Ineffective breathing pattern related to tracheobronchial obstruction.
- Risk for infection related to bacterial growth medium provided by pulmonary mucus and impaired body defenses.
- Imbalanced nutrition: less than body requirements related to impaired absorption of nutrients.
- Anxiety related to hospitalization.
- Compromised family coping related to child’s chronic illness and its demands on caregivers.
- Deficient knowledge of the caregiver related to illness, treatment, and home care.
Nursing Management
Nursing care of the adult with CF includes assisting the patient to manage pulmonary symptoms and to prevent complications of CF.
- Specific nursing measures include strategies that promote removal of pulmonary secretions; chest physiotherapy, including postural drainage, chest percussion, and vibration, and breathing exercises are implemented and are taught to the patient and to the family when the patient is very young.
- The patient is taught the early signs and symptoms of respiratory infection and disease progression that indicate the need to notify the primary health care provider.
- The nurse emphasizes the importance of an adequate fluid and dietary intake to promote removal of secretions and to ensure an adequate nutritional status. Because CF is a life-long disorder, patients often have learned to modify their daily activities to accommodate their symptoms and treatment modalities.
- Although gene therapy and double lung transplantation are promising therapies for CF, they are limited in availability and largely experimental. As a result, the life expectancy of adults with CF is shortened.
- For the patient whose disease is progressing and who is developing increasing hypoxemia, preferences for end-of-life care should be discussed, documented, and honored.
- Patients and family members need support as they face a shortened life span and an uncertain future.
Asthma
Asthma is a chronic inflammatory disorder of the airways associated with airway hyperresponsiveness that leads to recurrent episodes of wheezing, breathlessness, chest tightness and coughing. These episodes are usually associated with airflow obstruction within the lung, often reversible, either spontaneously or with treatment.
Factors that precipitate/aggravate asthma include: allergens, infection, exercise, drugs (aspirin), tobacco, etc.
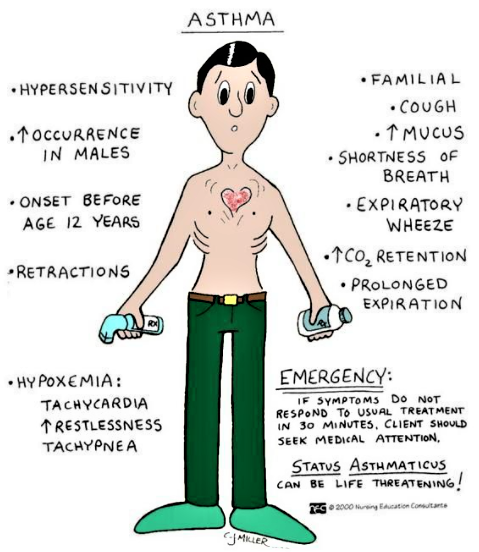
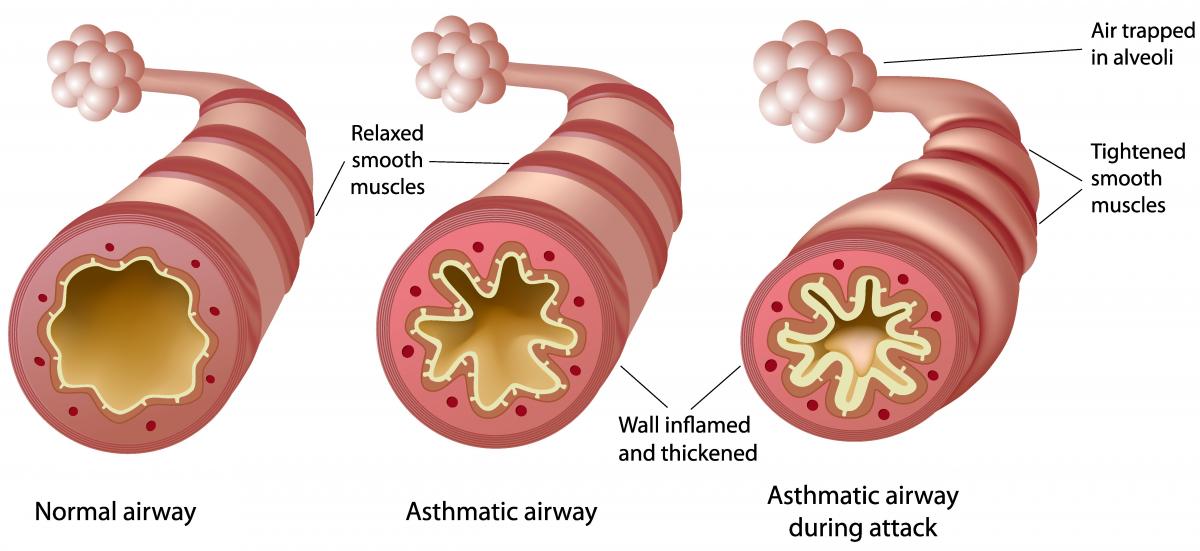
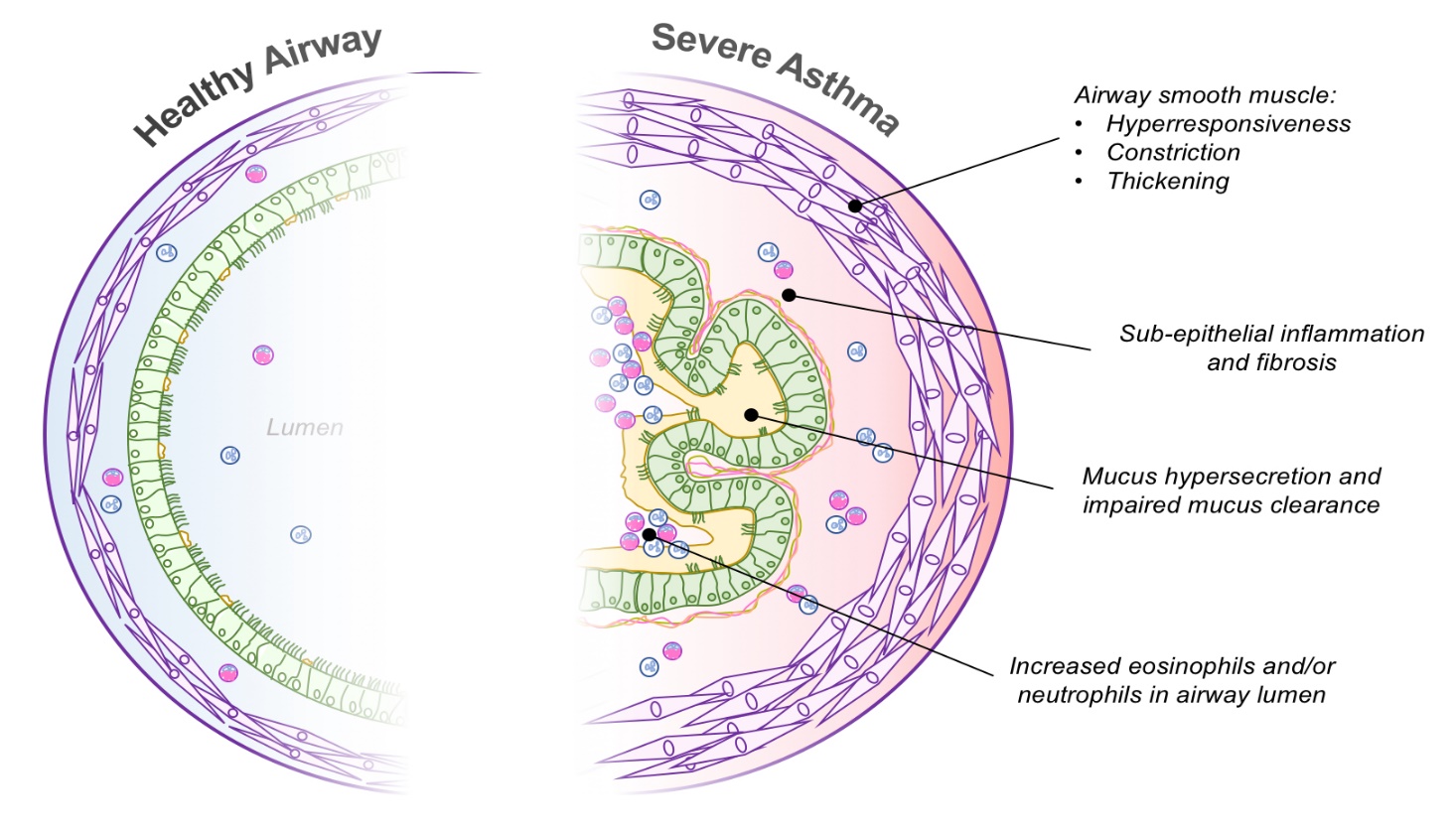
Pathophysiology:-
Airway inflammation is the primary problem in asthma. An initial event in asthma appears to be the release of inflammatory mediators triggered. The mediators are released from bronchial mast cells, alveolar macrophages, and epithelial cells. Some mediators directly cause acute bronchoconstriction.” The inflammatory mediators also direct the activation of eosinophils and neutrophils, and their migration to the airways, where they cause injury Called “late-phase asthmatic response” results in epithelial damage, airway edema, mucus hypersecretion and hyper responsiveness of bronchial smooth muscle varying airflow obstruction leads to recurrent episodes of wheezing, breathlessness, chest tightness and cough.
Causes/Triggers of Asthma:
The exact causes of asthma are still unknown but we do know that children are more likely to have asthma if other members of the family also have it. Related conditions like hay fever, eczema or food allergies can also increase the risk of asthma.
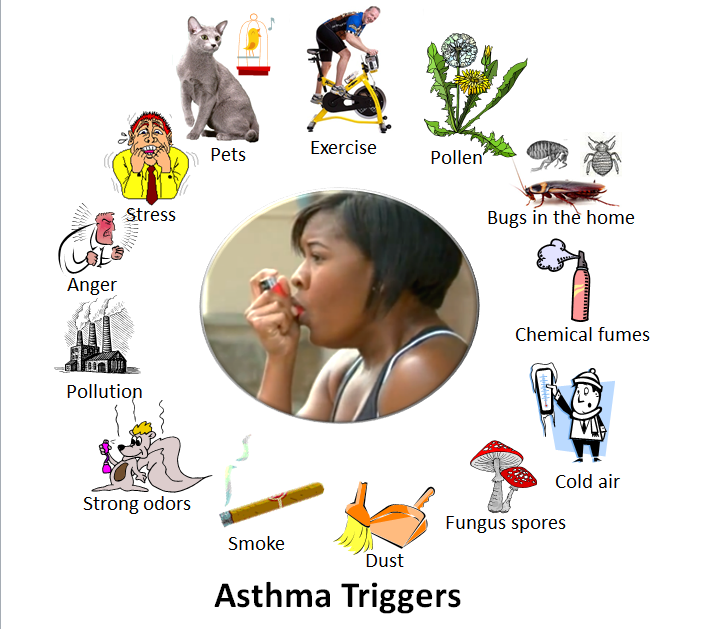 Smoking during pregnancy or exposing a child to tobacco smoke will increase their risk of developing asthma. Being overweight also increases the risk of developing asthma.
Smoking during pregnancy or exposing a child to tobacco smoke will increase their risk of developing asthma. Being overweight also increases the risk of developing asthma.
Though some children lose their symptoms as they grow older, asthma is a chronic disease so symptoms may come back later in life.
- Asthma is a breathing disease which is triggered by various allergies and substance, like:
- polluted matters, smoking, animal products and many more.
- Asthma problems can be caused by different foods which can react on the immune system of the body. Some people have allergy with particular food and various symptoms are appeared in your body like swelling, vomiting, diarrhea, rash, wheezing and breathing problems. The use of foods like peanuts, shellfish, eggs, various dairy products can be harmful for the patients so they should avoid all these foods. All such foods and wine containing histamine can cause development in asthma.
- The fizzy drinks, prepared salads and meats, home brewed beer and wine can contain the allergic reaction. If you have some problems of allergy, then you should contact with specialist for the allergic problems. The women can face the asthma problems during their periods, pregnancy, puberty and menopause.
The following things can trigger an asthma attack:
- Colds and Viral Infections
- House Dust Mites
- Fur and dander from pets
- Changes in weather, and cold air
- Pollen
- Tobacco smoke and pollution
- Mould
- Chemicals
- Allergies
- Exercise
Clinical Manifestations
The three most common symptoms of asthma are cough, dyspnea, and wheezing. In some instances, cough may be the only symptom. Asthma attacks often occur at night or early in the morning, possibly due to circadian variations that influence airway receptor thresholds.
- Cough. There are instances that cough is the only symptom.
- Dyspnea. General tightness may occur which leads to dyspnea.
- Wheezing. There may be wheezing, first on expiration, and then possibly during inspiration as well.
- Asthma attacks frequently occur at night or in the early morning.
- An asthma exacerbation is frequently preceded by increasing symptoms over days, but it may begin abruptly.
- Expiration requires effort and becomes prolonged.
- As exacerbation progresses, central cyanosis secondary to severe hypoxia may occur.
- Additional symptoms, such as diaphoresis, tachycardia, and a widened pulse pressure, may occur.
- Exercise-induced asthma: maximal symptoms during exercise, absence of nocturnal symptoms, and sometimes only a description of a “choking” sensation during exercise.
- A severe, continuous reaction, status asthmaticus, may occur. It is life-threatening.
- Eczema, rashes, and temporary edema are allergic reactions that may be noted with asthma.
Assessment of the severity of asthma attack
- The severity of the asthma attack must be rapidly evaluated by the following clinical criteria. Not all signs are necessarily present.
Assessment of severity in children over 2 years and adults
| Mild to moderate attack | Severe attack | Life threatening attack |
| to talk in sentences
Respiratory rate (RR) Children > 5 years ≤ 30/ minute Heart rate Children 2-5 years ≤ 140/ minute |
Cannot complete sentences in one breath or Too breathless to talk or feed RR Children 2-5 years > 40/minute Heart rate SpO2 ≥ 92% |
Altered level of consciousness (drowsiness, confusion, coma) Exhaustion
SpO2 < 92% |
Assessment and Diagnostic Findings
A complete family, environmental, and occupational history is essential.
- Positive family history. Asthma is a hereditary disease, and can be possibly acquired by any member of the family who has asthma within their clan.
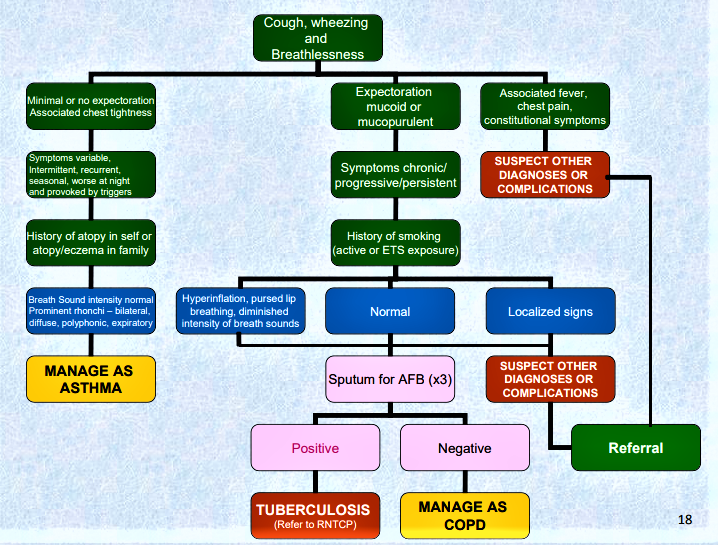
- Environmental factors. Seasonal changes, high pollen counts, mold, pet dander, climate changes, and air pollution are primarily associated with asthma.
- Comorbid conditions. Comorbid conditions that may accompany asthma may include gastroeasophageal reflux, drug-induced asthma, and allergic broncopulmonary aspergillosis.
Complications
Complications of asthma may include status asthmaticus, respiratoryfailure, pneumonia, and atelectasis. Airway obstruction, particularly during acute asthmatic episodes, often results in hypoxemia, requiring the administration of oxygen and the monitoring of pulse oximetry and arterial blood gases. Fluids are administered because people with asthma are frequently dehydrated from diaphoresis and insensible fluid loss with hyperventilation.
Medical Management
Immediate intervention is necessary because the continuing and progressive dyspnea leads to increased anxiety, aggravating the situation.
Goals of Asthma Therapy
- Prevent recurrent exacerbations and minimize the need for emergency department visits or hospitalizations
- Maintain (near‐) “normal” pulmonary function
- Maintain normal activity levels (including exercise and other physical activity)
- Provide optimal pharmacotherapy with minimal or no adverse effects
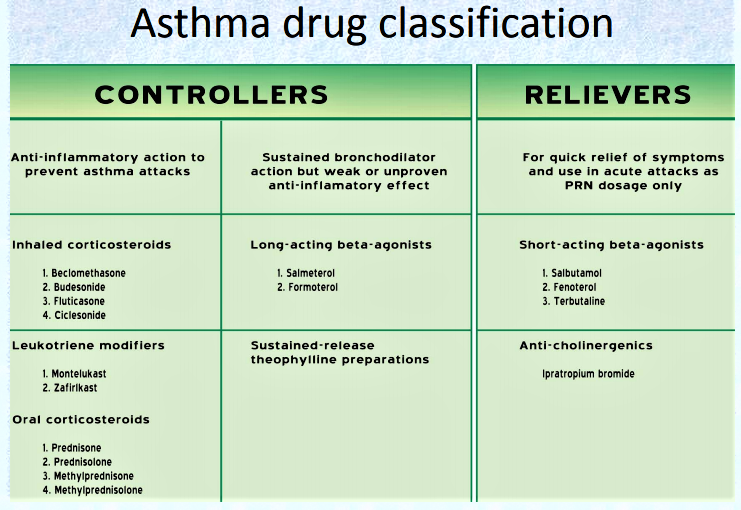
Pharmacologic Therapy
There are two classes of medications—long-acting control and quick-relief medications—as well as combination products.
- Short-acting beta2-adrenergic agonists
- Anticholinergics
- •Corticosteroids: metered-dose inhaler (MDI)
- Leukotriene modifiers inhibitors/antileukotrienes
- Methylxanthines
Mild to moderate attack
– Reassure the patient; place him in a 1/2 sitting position.
– Administer:
• salbutamol (aerosol): 2 to 4 puffs every 20 to 30 minutes, up to 10 puffs if necessary during the first hour. In children, use a spacer 1to ease administration (use face mask in children under 3 years).
Single puffs should be given one at a time, let the child breathe 4 to 5 times from the spacer before repeating the procedure.
• prednisolone PO: one dose of 1 to 2 mg/kg
– If the attack is completely resolved: observe the patient for 1 hour (4 hours if he lives far from the health centre) then give outpatient treatment: salbutamol for 24 to 48 hours (2 to 4 puffs every 4 to 6 hours depending on clinical evolution) and prednisolone PO (1 to 2 mg/kg once daily) to complete 3 days of treatment.
– If the attack is only partially resolved, continue with salbutamol 2 to 4 puffs every 3 to 4 hours if the attack is mild; 6 puffs every 1 to 2 hours if the attack is moderate, until symptoms subside, then when the attack is completely resolved, proceed as above.
– If symptoms worsen or do not improve, treat as sever attack.
Severe attack
– Hospitalise the patient; place him in a 1/2 sitting position.
– Administer:
• oxygen continuously, at least 5 litres/minute or maintain the SpO2 between 94 and 98%.
• salbutamol (aerosol): 2 to 4 puffs every 20 to 30 minutes, up to 10 puffs if necessary in children under 5 years, up to 20 puffs in children over 5 years and adults. Use a spacer to increase effectiveness, irrespective of age.
or salbutamol (solution for nebulisation), see Life-threatening attack
• prednisolone PO: one dose of 1 to 2 mg/kg
In the case of vomiting, until the patient can tolerate oral prednisolone, use hydrocortisone IV:
Children 1 month to < 5 years: 4 mg/kg every 6 hours (max. 100 mg per dose)
Children 5 years and over and adults: 100 mg every 6 hours
– If the attack is completely resolved, observe the patient for at least 4 hours. Continue the treatment with salbutamol for 24 to 48 hours (2 to 4 puffs every 4 hours) and prednisolone PO (1 to 2 mg/kg once daily) to complete 3 days of treatment.
Reassess after 10 days: consider long-term treatment if the asthma attacks have been occurring for several months. If the patient is already receiving long-term treatment, reassess the severity of the asthma (see table) and review compliance and correct use of medication and adjust treatment if necessary.
– If symptoms worsen or do not improve, see Life-threatening attack.
Life-threatening attack (intensive care)
– Insert an IV line.
– Administer:
• oxygen continuously, at least 5 litres/minute or maintain the SpO2 between 94 and 98%.
• salbutamol + ipratropium nebuliser solutions using a nebuliser:
| Children 1 month to < 5 years | salbutamol 2.5 mg + ipratropium 0.25 mg every 20 to 30 minutes |
| Children 5 to < 12 years | salbutamol 2.5 to 5 mg + ipratropium 0.25 mg every 20 to 30 minutes |
| Children 12 years and over and adults | salbutamol 5 mg + ipratropium 0.5 mg every 20 to 30 minutes |
The two solutions can be mixed in the nebuliser reservoir.
• corticosteriods (prednisolone PO or hydrocortisone IV) as for severe attack
– If the attack is resolved after one hour: switch to salbutamol aerosol and continue prednisolone PO as for severe attack
– If symptoms do not improve after one hour:
• administer a single dose of magnesium sulfate by IV infusion in 0.9% sodium chloride over 20 minutes, monitoring blood pressure:
Children over 2 years: 40 mg/kg
Adults: 1 to 2 g
• continue salbutamol by nebulisation and corticosteriods, as above.
Notes:
– In pregnant women, treatment is the same as for adults. In mild or moderate asthma attacks, administering oxygen reduces the risk of foetal hypoxia.
– For all patients, irrespective of the severity of the asthma attack, look for underlying lung infection and treat accordingly.
If a conventional spacer is not available, use a 500 ml plastic bottle: insert the mouthpiece of the inhaler into a hole made in the bottom of the bottle (the seal should be as tight as possible). The child breathes from the mouth of the bottle in the same way as he would with a spacer. The use of a plastic cup instead of a spacer is not recommended (ineffective).
Nursing Management
The immediate nursing care of patients with asthma depends on the severity of symptoms. The patient and family are often frightened and anxious because of the patient’s dyspnea.
Therefore, a calm approach is an important aspect of care.
- Assess the patient’s respiratory status by monitoring the severity of symptoms, breath sounds, peak flow, pulse oximetry, and vital signs.
- Obtain a history of allergic reactions to medications before administering medications.
- Identify medications the patient is currently taking.
- Administer medications as prescribed and monitor the patient’s responses to those medications; medications may include an antibiotic if the patient has an underlying respiratory infection.
- Administer fluids if the patient is dehydrated.
- Assist with intubation procedure, if required.
Promoting Home- and Community-Based Care
Teaching Patients Self-Care
- Teach patient and family about asthma (chronic inflammatory), purpose and action of medications, triggers to avoid and how to do so, and proper inhalation technique.
- Instruct patient and family about peak-flow monitoring.
- Teach patient how to implement an action plan and how and when to seek assistance.
- Obtain current educational materials for the patient based on the patient’s diagnosis, causative factors, educational level, and cultural background.
Continuing Care
- Emphasize adherence to prescribed therapy, preventive measures, and need for follow-up appointments.
- Refer for home health nurse as indicated.
- Home visit to assess for allergens may be indicated (with recurrent exacerbations).
- Refer patient to community support groups.
- Remind patients and families about the importance of health promotion strategies and recommended health screening.
First Aid
Wound: Abnormal break in skin which permits the escape of blood, and may allow the entrance of germs, causing infection.
Types of Wound:
- Incise Wound – Clean cut caused by sharp instrument.
- Laceration Wound – Jagged cut or tear caused by sharp irregular edges.
- Contusion – Caused by blunt instrument / fall against hard surface. Skin is not broken.
- Abrasion – Simple scrapes and scratches usually from a sliding fall.
- Puncture Wound – Penetrating wound by sharp, pointed instrument. Can result in serious internal injury.
- Stab Wound – Caused by a bladed object.
- Gun Shot Wound
Ways to Stop Bleeding:
- Direct pressure
- Indirect pressure
- Elevation
Wound Management:
Slight Bleeding
-Wash your hands and wear a pair of gloves.
– Rinse wound with running water.
– Dab gently to dry.
– Apply direct pressure or elevation if bleeding still occurs.
– Cover wound with sterile swab.
– Clean surrounding area of skin with water and soap.
– When cleaning, wipe away from wound and use each swab only once.
– Avoid wiping away blood clots.
– Pat dry.
– Dress wound with adhesive dressing.
Severe Bleeding
Aim of managing severe bleeding: a) control bleeding b) minimize risk of infection
– Lay casualty down to prevent shock.
– Support injured part.
– Send to hospital.
– Wash hands.
Bandaging:
- Triangular bandage (Reef Knot – L over R; R over L)
- Broad bandage
- Narrow bandage
Slings and Bandaging:
- Simple sling
- Elevated sling
- Scalp bandage
- Palm bandage
- Fist bandage
Fracture: A break or crack in the bone caused by direct force and indirect force.
Type:
- Closed or simple fracture (no wound)
- Open or compound fracture (wound is present)
- Comminuted (totally crushed)
- Green stick injury (In children; mixture of bend and break)
- Unstable fracture
Management of Closed Fractures:
- Do not move the casualty until you support the injured part.
- Steady and support the injured part.
- Immobilize the injured part using bandages and slings.
- Elevate the injured part.
- Treat for shock if possible.
- Check circulation every 10 minutes.
- Send to hospital.
- Do not give him anything to eat or drink.
Management of Open Fractures:
- Cover wound with sterile / clean dressing.
- Control bleeding.
- If wound is jutting, place padding.
- Immobilize the injured part.
Dislocation: Displacement of a bone at a joint caused by strong force, wrenching the bone into an abnormal position or violent muscle contraction.
Sprain: Injury to a ligament at or near a joint frequently caused by wrenching movement at joint that tears the surrounding tissue.
Strains: Partial tearing of the muscles at the junction of muscle and tendon that joins it to a bone.
Management of Sprain and Strains (Soft Tissue Injury):
| R | Rest |
| I | Ice – Reduce swelling |
| C | Compression |
| E | Elevation |
If injury is very bad, send the casualty to the hospital.
Cramps: Sudden, involuntary and painful muscle spasm.
Cramp in Foot:
- Ask casualty to stand on toes.
- Massage foot with fingers.
Cramp in Calve:
- Straighten the knee.
- Draw the foot firmly and steadily upwards towards the shin.
- Massage.
Cramp in Back of Thigh:
- Straighten the knee by raising his leg.
- Massage the muscles.
Cramp in Front of Thigh:
- Bend knee.
- Massage muscles slowly.
Signs & Symptoms:
- Difficult to move a limb
- Pain near the site of injury
- Tenderness
- Distortion
- Swelling
- Bruising
- Shortening, bending or twisting of the limb
- Crepitus (sound) caused by grating of the bone end
Lifting and Moving Casualty
Rules:
- Do not move casualty unless absolutely necessary.
- Explain to casualty what you are doing.
- Never move casualty alone.
- Instruct helpers what they are supposed to do.
- Protect yourself using the correct techniques.
- Ensure casualty’s safety.
Correct Lifting Techniques:
- Place feet comfortably apart, one slightly in front of the other.
- Keep back straight.
- Bend your knees.
- Grip with both hands.
- Keep weight of person you are lifting as close to you as possible.
Lifting Method:
Casualty is conscious and able to walk:
- Use the human crutch
Casualty is conscious but unable to walk:
- Pick-a-back
- Drag method
- 4 handed seat
- 3 handed seat
- 2 handed seat
- Fore & aft
- Carry chair
Casualty is unconscious:
- Cradle method
- Drag method
- Fore & aft
- Stretcher method
Pediatrics Nursing Paper/MCQs
Basis of Pediatrics Nursing
Student Name: ___________S/O_____________ Roll No: ________
Maximum Marks: 100 Passing Marks: 50 Time: 3 Hours Date:
A. OBJECTIVE SECTION
MCQs
Note: Circle the one best answer.
- Which cell type is responsible for the early asthmatic response?
- Basophil
- Eosinophil
- Mast cell
- Neutrophil
- Congenital cyanotic heart disease includes:
- VSD.
- Patent Ductus Arteriosus.
- Fallot tetralogy.
- ASD
- Fallot tetralogy include:
- Pulmonary stenosis
- Ventricular septal defect
- Over riding aorta
- All of the above
- Serious complications of Fallot tetralogy includes
- Eisenminger syndrome
- Recurrent pneumonia
- Brain abscess
- Pulmonary hypertension
- Major manifestations of Rheumatic fever include all the following, Except:
- Carditis
- Arthralgia
- Chorea
- Erthema nodosa
- All the following are true about acute bronchiolitis, Except:
- Most cases are under two years old.
- Most cases are caused by respiratory syncytial virus.
- Antibiotics are recommended in infants below three months age.
- Steroids maybe helpful in some cases.
- Bronchial asthma is characterized by all the following, Except:
- Hyper active air way
- Clubbing
- Spasmodic cough
- Bilateral chest wheezes
- All of the following cause acute wheezing, Except:
- Bronchitis
- Bronchiolitis
- Bronchiaectasis
- Bronchial asthma
- All of the following are common causes of bacterial pneumonia, Except:
- Staphylococci.
- Hemophillus influenza.
- Pseudomonas.
- Klepsiella.
- All of the following are common causes of empyema, Except:
- Staphylococcal pneumonia
- Lung abscess
- Measles
- Chest injury
- The organ of gas exchange in the fetus is the
- Amniotic fluid
- Umbilical cord
- Placenta
- Lungs
- Commonest cause of bacterial pneumonia in infancy:
- H.. influenza
- Streptococcus
- Staphylococcus
- Pneumococcus
- Serious complications of staphylococcal pneumonia include all the following Except :
- Lung abscess
- Bronchitis
- Empyema
- Lung collapse
- Asthma triggers include all the following Except :
- Viral respiratory infections
- Tobacco smoke
- House dust mite
- Steroids
- Which of the following statement is not true about Breast milk
- It contains carbohydrates 7.0 gm %.
- It contains proteins 4.0 gm %.
- It contains water 87.5 %.
- It contains less calcium than cow milk.
- Non nutritional marasmus may be caused by.
- Acute gastroenteritis.
- Staphylococcal pneumonia.
- V.S.D.
- Urinary tract infections
- All the following are causes vitamin D deficiency rickets, Except:
- Low calcium in diet.
- Prolonged breast feeding
- Lack of sun exposure.
- Non response of bone receptors to vitamin D
- Colostrum is privileged by having.
- High iron.
- High antibodies.
- High vitamin D.
- High calcium
- The important reflex necessary for breast feeding:
- Moro reflex
- Grasp reflex
- Rooting reflex
- Cough reflex
- The clinical signs of kwashiorkor include the following, Except:
- Edema
- Skin changes
- Hair changes
- Bone changes
- The complications of rickets include all of the following, Except:
- Tetany
- Tetanus
- Respiratory infection
- Fractures
- Breast milk contains all of the following nutritional constituents, Except:
- 7.2 gm fats
- l.2 gm proteins
- 7.0 gm carbohydrates
- 87.5% water
- A fourth degree marasmus infant is characterized by .
- Loss of buccal pad of fats.
- Skin changes
- Edema.
- Bowed legs
- Breast milk contains all of the following nutritional constituents, Except:
- 3.5 gm fats
- 1.2 gm proteins
- 3.5gm carbohydrates
- 87.5% water
- Recommended basic requirement of vitamin D for infants is:
- 400 u Ikg
- 800 ulkg
- 200 ulkg
- 100 u/kg
- Breast milk in the first three days after delivery shows all the following, Except:
- Called colostrum
- Rich in proteins
- High vitamin K content
- High caloric value
- The clinical signs of kwashiorkor include the following except
- Edema
- Skin changes
- Hair changes
- Bone changes
- Colostrum is Breast milk secreted in the first post-natal :
- 2-3 days
- One week.
- 3-5 days
- One month
- Which of the following is not a compulsory vaccine given in the first year of life:
- Measles Vaccine.
- BCG Vaccine.
- Meningitis vaccine.
- Polio vaccine.
- All the following infectious diseases are essentially associated with rash, Except:
- German measles.
- Chickenpox.
- Mumps.
- Roseola infantum
- The incubation period of chickenpox is:
- One week
- 2 to 3 weeks
- 2 to 3 months
- 3 days
- Oral polio vaccine is.
- Live attenuated vaccine.
- Killed vaccine.
- Given at birth.
- Given at 4,8,12 months of age
- Paroxysmal stage of pertussis persists for:
- 2 weeks
- 4 weeks
- 3 weeks
- 8 weeks
- The incubation period of measles is :
- 2 weeks
- 4 weeks
- 3 weeks
- 8 weeks
- The incubation period of Chickenpox is :
- 3 weeks
- 4 weeks
- 8 weeks
- 1 week
- Rash of measles is characterized by all the following Except:
- Starts behind the ears.
- Spread from above downwards
- May be hemorrhagic in immunocompromised children
- May be vesicular
- The manifestations of rubella syndrome include the following except
- Mental retardation
- Microcephaly
- Cardiac defects
- Macrocephaly
- The virus causing chicken pox
- Rubella
- Varicella
- Herpes simplex
- None
- Paroxysmal stage of pertussis persists for :
- 2 weeks
- 3 weeks
- 4 weeks
- 6 weeks
- Measles rash begins :
- On chest and back
- Behind ear
- Behind neck
- On the face
- Complications of diphtheria include all the following Except :
- Squint
- Flaccid paraplegia
- Heart failure
- Ataxia
- The most common cause of hypovolemic shock is .
- Acute renal failure.
- Heart failure.
- Gastro enteritis.
- Toxic. coma
- The most common cause for recurrent abdominal pains in children is.
- Renal stones.
- Familial Mediterranean fever
- Intestinal parasites.
- Inflammatory bowel disease.
- Serious complications of gastroenteritis include:
- Dehydration
- Acidosis
- Shock
- All of the above
- Hypertonic dehydration is characterized by:
- Moist tongue
- Lost skin elasticity
- High serum sodium
- Drowsiness
- All of the following are correct about physiological jaundice, Except:
- It is a conjugated hyperbilirubinemia
- The baby looks healthy and feeds well
- Doesn’t exceed 12 mg/dl
- It doesn’t persist more than 7 days
- All of the following are true about phototherapy, Except:
- Reduce serum unconjugated bilirubin level.
- Can cause watery stools.
- Increase fluid requirement.
- Can be a substitute for Exchange transfusion in small preterm with hyperbilirubinemia.
- Neonatal period extends up to:
- 21 days.
- 28 days.
- 30 days.
- 35 days.
- Moro reflex in normal neonates disappear at
- 1 week
- 3 weeks
- 6 weeks
- 3 months
- The umbilical cord contains
- One artery and one vein
- One artery and two capillaries
- Two arteries and one vein
- Two veins and one artery
- Persistence of Moro reflex at 12 weeks indicate :
- Brain damage
- Normal child
- Hungry child
- Irritable child
- Atelectasis due to intra-bronchial obstruction may be due to:
- Foreign body
- Mucus plug
- Both
- None
- Common presentations of chronic renal failure in children include :
- Anemia
- Bone deformity
- Hypertension
- All of the above
- The cause of death in spinal polio is:
- Paralysis of respiratory muscles
- Cardiac arrest
- Cranial nerve paralysis
- Urinary complications
- All of the following might be causes of cerebral palsy ,Except:
- Kernicterus.
- Toxoplasmosis.
- Congenital hypothyroidism.
- Tuberous sclerosis
- Cerebral palsy is characterized by
- Mental retardation
- Motor disability
- Curable
- Sensory loss
- The fatal poliomyelitis is :
- Bulbar polio
- Spinal polio
- Encephalitis
- Cerebral polio
- Delayed puberty may be due to:
- Growth hormone deficiency
- Malnutrition
- Hypothyroidism
- All of the above
- The site of lesions in myasthenia gravis:
- Spinal cord
- Neuromuscular junction
- Cranial nerves
- All of the above
- An infant sits without support by….. Month.
- 5 month.
- 7 month.
- 8 month.
- 9 month.
- The head circumference ,by the end of the second year equals:
- 35 cm.
- 45 cm.
- 50 cm.
- 60 cm .
- Infants body weight is tripled by the age of:
- 5 months
- 24 months
- 12 months
- 18 months
- Short stature may be due to:
- Growth hormone deficiency
- Malnutrition
- Hypothyroidism
- All the above
- An infant supports his head by … … months
- 2 months
- 4 months
- 8 months
- 10 months
- Weight gain in the first four months of age increase by
- 250 gm/month.
- 500 gm/ month
- 800 gm/ month
- 1500 gm/ month
- Grasp reflex in normal neonates is present since.
- 1 week
- 3 weeks
- Birth
- 3 months
- The first deciduous tooth appears by
- 3-4 months
- 4-5 months
- 8-9 months
- 5-7 months
- The faster weight gain is seen at
- First year and puberty
- Second year and puberty
- Puberty
- Infancy
- A child starts crawling
- 5 months
- 7 months
- 8 months
- 9 months
- The average monthly weight gain in the first 4 months :
- 250 gm.
- 500 gm.
- 750 gm.
- 1000 gm
B. Read each statement carefully and circle the correct answer as true or false. (10 Marks)
- Humans serve as a reservoir for meningococcal meningitis.
- True
- False
- Currently there is no vaccine for meningococcus.
- True
- False
- Tetanus is nearly always fatal.
- True
- False
- Viral meningitis (“aseptic meningitis”) is usually far more severe and deadly than bacterial or fungal meningitis.
- True
- False
- The common cold is caused by one virus.
- True
- False
- Mycobacterium tuberculosis can survive up to 10 years suspended in fine aerosols.
- True
- False
- Meningitis refers to inflammation of the brain.
- True
- False
- Is meningitis contagious?
- True
- False
- Spina bifida is the deformity of the brain.
- True
- False
- Cleft lip and palate occurs always unilaterally.
- True
- False
SUBJECTIVE SECTION (20 Marks)
Attempt any five of the following questions. All questions carry equal marks.
Q.No. 01 List the causes of birth defects and explain any one of them: (04 Marks)
____________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________
Q.No. 02 Define the Mylomeningocele along with sign and symptoms. (04 Marks)
____________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________
Q.No. 03 Write 10 most common accidents of children age with their preventive measures. (04 Marks)
____________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________
Q.No. 04 Define tetanus. Explain nursing management of tetanus case. (04 Marks)
______________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________
Q.No. 05 Enlist the responsibilities of a pediatric nurse. (04 Marks)
______________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________
Q.No. 06 Write down the difference between diarrhea and dysentery. (04 Marks)
______________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________Q.No. 07 Define Down Syndrome and elaborate its nursing management. (04 Marks)
__________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________
………..THE END………….
Gastro Intestinal System
Gastro-intestinal system
Gastro-intestinal tract
The Gastro-intestinal Tract is also termed as Digestive System and alimentary canal, consists of GI Tract and its accessory organs. The GI Tract is a hollow muscular tube that extends from mouth o anus. Its principal function is to provide the body with fluids, nutrients and electrolyte. This is accomplished through the process of ingestion (taking alcohol), digestion (breakdown of food) and absorption (transfer of food into circulation). Another main function of GI system is the storage and final excretion of solid waste products of digestion i.e.: elimination.
| Location of organs in each abdominal Quadrant | |||
| 1. | Right upper Quadrant (RUQ) | 2. | Right lower Quadrant (RLQ) |
| § | Liver | · | Caecum |
| § | Gall bladder | · | Appendix |
| § | Duodenum | · | Right ovary & tube |
- Right Kidney
- Hepatic flexure of colon
| 3. | Left upper Quadrant (LUQ) | 4. | Left lower Quadrant (LLQ) |
| § | Stomach | · | Sigmoid colon |
| § | Spleen | · | Left ovary & tube |
- Left Kidney
- Pancreas
- Splenic flexure of colon
- Esophageal Carcinoma
Definition:
Carcinoma of the esophagus is unique in its geographic distribution. Both benign & malignant tumor occurs in the esophagus. Benign tumor are usually leimyomas, and extremely rare & usually asymptomatic. They require no intervention unless symptoms necessitate local excision. Malignant tumors of the esophagus are not common but they assume increased importance because of their virulence.
Location of esophagus:
Esophagus lies behind the trachea to which it adopts and in front of the vertebral column. Passing through the thorax it pierces the diaphragm to enter in abdomen where it communicates with the stomach. Its size is 9-10 inches.
Causes:
- Exact cause is idiopathic,
- Pre-disposing factors are:
- Taking alcohol
- Usage of tobacco and opium
- Excessive usage of beverages
- Induced caustic esophagus sphincter
- Ultra-violet radiations
Sign and Symptoms
- Tumor
- Dysphagia
- Odynophagia (typically)
- Heart burn
- Anorexia
- Weight loss
- Feeling mass in throat
- Painful swallowing
- Regurgitation
- Hiccup
- Chest pain
- Supera-clavicular lymphodenopathy
Complication:
- Hemorrhage
- Esophageal perforation
- Esophageal obstruction
Investigations:
- Chest X-ray
- CT scan
- Barium esophagography
- Bronchoscopy
- Biopsy
- MRI
- Blood CP
Medical treatment:
- Poly-functional alkyl ting agents:
- Antimetabolytes:
- e.g.: Folic acid, purine antagonistic
- ACTH
- Castration
- Miscellaneous drugs:
- Antibiotics drugs such as Actinomycin-D, Mytomycin
Surgical treatment:
- Surgical, the resection of the esophagus provides the most rapid durable relief of the Dysphagia, the standard surgical Management including partial removal of the esophagus.
- Esophagectomy
- Esophagogastrotomy
- Esophagoenterostomy
Radio-therapy:
- The radiotherapy may be given for a short time to provide relief to pain. Nursing Management:
- Please revise the general Nursing Management of the Neoplasm.
Peptic Ulcer
Definition:
Peptic (Stomach + Duodenum) ulcer is an erosion of the Gastro-intestinal (GI) mucosa resulting from the digestive action of HCl and pepsin.
- HCl is produced by stomach parietal cells.
- Pepsin produced by___________________
Duodenal ulcer is common than gastric ulcer.
Classification of PUD:
Classification depends upon degree of the mucosal involvement & gastric or duodenal
Acute Ulcer:
Acute associated with superficial erosion & minimal inflammation. It is short-duration & resolves quickly when the cause is identified & removed.
Chronic Ulcer:
A long duration, eroding through the muscular wall with the formation of fibrous tissue. It is present continuously for many months or intermitely throughout the person’s life time. A chronic Ulcer is at least four times as common as acute erosions.
Difference between Gastric Ulcer & Duodenal Ulcer
| No: | Gastric Ulcer | Duodenal Ulcer |
| 1 | Lesion: | Lesion: |
| Superficial, Smooth, Round shape | Deep, Bulb shape (1-2 cm) | |
| 2 | Gastric Secretion: | Gastric Secretion: |
| Increase, More found in women | Increase, More found in men | |
| 3 | Clinical features: | Clinical features: |
| Burning, Pain 1-2 hour after meal | Burning, Cramping, pain 2-4 hours | |
| after meal | ||
| 4 | Pain: | Pain: |
| Left Epigastric region, often retrieved | Mid-epigastria region, often not relieved | |
| by food | by food |
Causes:
- Idiopathic but Helico pylori bacterium is the major cause, and risk factors are:
- Smoking
- Stress
- Alcohol
- Excessive secretion of the HCl
- Heredity (Blood Group O)
- Hurry, Worry & Curry
- NSAID
Types of Peptic Ulcer:
- Gastric Ulcer
- Duodenal Ulcer
- Esophageal Ulcer
- Joudjenal Ulcer
Sign and Symptoms
- Epigastria pain
- Discomfort
- Vomiting (Gastric Ulcer)
- Weight loss (Gastric Ulcer)
- Weight gain (Duodenal Ulcer)
- Hunger (Duodenal Ulcer)
- Epigastria tenderness
- Dyspepsia
- Diaphoresis
- Constipation
- Endoscopy (Gastro scopy)
- Barium radiotherapy
- Biopsy
- Barium meal X-ray
- Blood CP
- Blood ESR
- Hemorrhage
- Perforation
- Pyloric stenosis
- Malignant Chance
- Gastric-intestinal obstruction
- Meal should be taken at regular interval
- Hurry, Worry, Curry, Spicy, Fry, Vinegary food should be avoided
- Avoid alcohol, smoking and beverages
- NSAID discontinues
- Syp: MOM
- Syp: Simeco
- Syp: Cremafin
H2 antagonistic receptors
- Tab: Zantac 150mg
- Tab: Anzol
- Cap: Zoton
- Cap: Benzin
Bosom pump inhibitor (more effective than H2 receptors)
- Omeprazole
- Pentaprazole
- Famotidine at night for 24 weeks
- Tab: Flodin
- Tab: Famodin
- Tab: Peptin Antibiotics
- Tab: Amoxicillin
If Medical therapy fails to heal, surgery is managed for the patient if chances of complications are.
- Partial gastrectomy
- Vagotomy
- Pyloroplasty
Nursing Management:
- Recumbent position should be maintained to prevent from severe hemorrhage
- Advised for left-lateral position for 20-30 minutes after eating
- Avoidance from alcohol, beverages, tobacco & spicy food
- Advice for small frequent meals
- Administration of anti-cholergic or anti-spasmodic medication as prescribed by the physician
- Maintain I/O chart
- TPR & BP should be monitored
- Tachyponea may occur due to loss of blood
- Provide psychological support
- Health education
- Observe for vomiting
- Assess for faintness
