Introduction:
Appendicitis is an inflammation of the appendix.
It is a medical emergency that usually leads to removal of the appendix before it can rupture, as this can cause infection and even death.
Surgically removing the appendix appears to have no effect on the digestive system.
Appendicitis can occur at any age but usually affects children and young adults.
Appendicitis is found on the right lower side of the abdomen and connects to the cecum of the large intestine. It looks like a protruding worm or finger-like structure coming out of the large intestine, specifically the ascending colon.
The role of the appendix: it plays a role in storing the “good” bacteria in your GI tract while the tract is recovering from a diarrhea illness (so it helps maintain healthy GI flora.
Types of Appendicitis
The two types of appendicitis depending on the onset, which are:
- Acute Appendicitis – It develops very fast within a few days to hours, and requires prompt medical treatment or surgery.
- Chronic Appendicitis – Here, the inflammation lasts for a long time. It is a rare condition.
And depending on the complications:
- Simple Appendicitis – Cases with no complications.
- Complex Appendicitis – Cases that involve complications like appendix rupture or abscess.
Causes
The exact causes are not clear, but it usually involves:
- a blockage of the lumen of the appendix (leading to increased pressure and impaired bloodflow, which results in inflammation).
- This is usually caused by faeces, but bacterial or viral infections in the digestive tract can lead to swelling of lymph nodes (lymphoid hyperplasia), which puts pressure on the appendix and causes obstruction.
- Untreated, the appendix can become gangrenous or rupture. If it ruptures, the infection may be released into the abdomen.
- inflammatory bowel disease.
- stool, parasites, or growths that can clog your appendiceal lumen.
- trauma to your abdomen.
Pathophysiology
Appendicitis occurs when the appendix becomes acutely inflamed. It’s not entirely known why appendicitis occurs however it is thought to be due to the lumen of the appendix becoming blocked by a faecolith, normal faecal matter or lymphoid hyperplasia due to a viral infection.
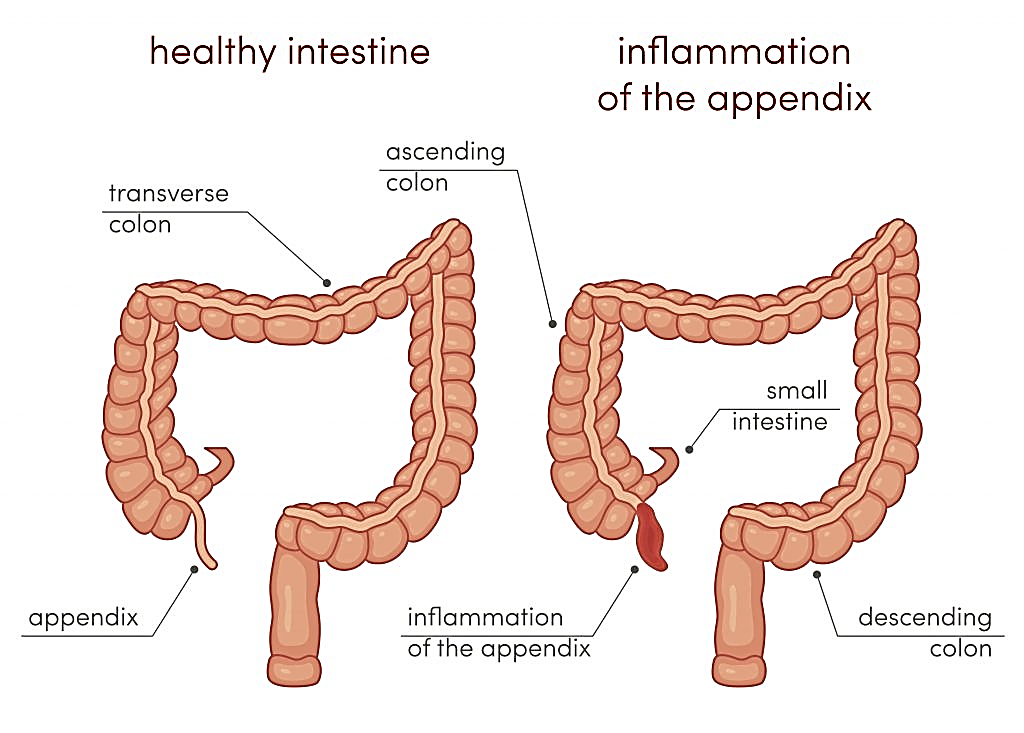 Once obstructed, there is reduced blood flow to the tissue and bacteria is able to multiply. Due to the lumen being obstructed, the pressure within the appendix increases and this reduces venous drainage, resulting in ischaemia. If untreated the ischaemia can lead to necrosis and gangrene. At this stage, the appendix is at risk of perforating. It takes around 72hrs for perforation to occur from when the appendix becomes obstructed. Once the appendix perforates, bacteria and inflammatory cells are released into the surrounding structures. This then causes inflammation of the peritoneum and the child develops peritonitis causing diffuse abdominal pain.
Once obstructed, there is reduced blood flow to the tissue and bacteria is able to multiply. Due to the lumen being obstructed, the pressure within the appendix increases and this reduces venous drainage, resulting in ischaemia. If untreated the ischaemia can lead to necrosis and gangrene. At this stage, the appendix is at risk of perforating. It takes around 72hrs for perforation to occur from when the appendix becomes obstructed. Once the appendix perforates, bacteria and inflammatory cells are released into the surrounding structures. This then causes inflammation of the peritoneum and the child develops peritonitis causing diffuse abdominal pain.
Signs and Symptoms of Appendicitis
Remember “Appendix”
- Abdominal pain (will be dull at first with pain at or around the belly button that radiates to the right lower quadrant and it will localize at this spot)
- Point of McBurney’s will have the most pain (found one-third distance between the belly button and anterior superior iliac spine)
- Poor appetite
- Elevated temperature
- Nausea/vomiting
- Desire to be in the fetal position to relieve pain (side lying with knees bent)
- Increased WBC, inability to pass gas or have a bowel movement (constipation..can have diarrhea too)
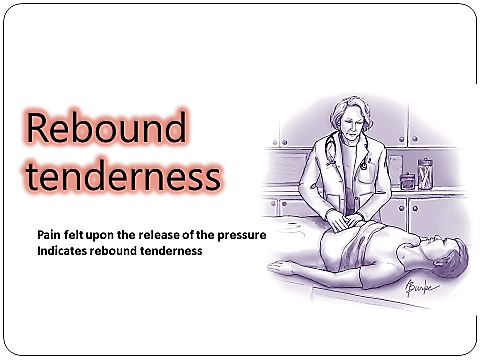
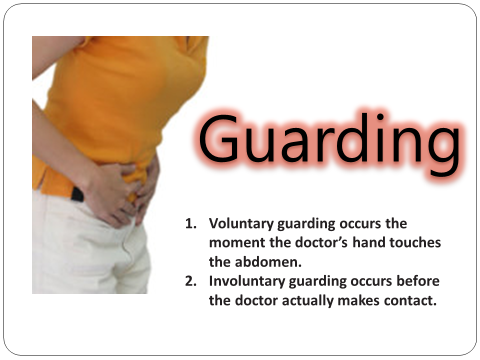
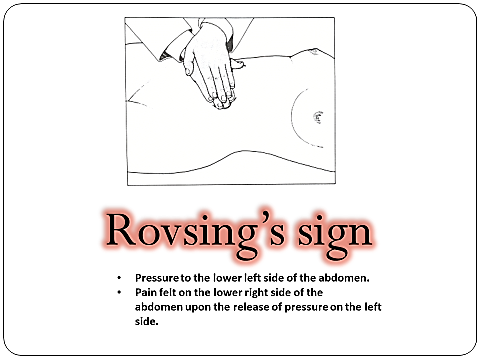
- eXperiences rebound tenderness (when pressure is applied to the right lower quadrant it hurts but it HURTS MORE when the pressure is released) and abdominal rigidity on palpation (involuntary stiffening of the abdominal muscle when abdomen palpated).
Complications
If appendicitis is left untreated, a complication could occur.
Perforation of the appendix. This is a major complication of appendicitis, which can lead to peritonitis, abscess formation, or portal pylephlebitis.
Perforation generally occurs 24 hours after the onset of pain.
Symptoms include a fever of 37.7⁰C or greater, a toxic appearance, and continued abdominal pain or tenderness.
Assessment and Diagnostic Findings
Diagnosis is based on the results of a complete physical examination and on laboratory findings and imaging studies.
- CBC count: A complete blood cell count shows an elevated WBC count, with an elevation of the neutrophils.
- Imaging studies: Abdominal x-ray films, ultrasound studies, and CT scans may reveal a right lower quadrant density or localized distention of the bowel.
- Pregnancy test: A pregnancy test may be performed for women of childbearing age to rule out ectopic pregnancy and before x-rays are obtained.
- Laparoscopy: A diagnostic laparoscopy may be used to rule out acute appendicitis in equivocal cases.
- C-reactive protein: Protein produced by the liver when bacterial infections occur and rapidly increases within the first 12 hours.
Medical Management
Medical management should be performed carefully to avoid altering the presenting symptoms.
- IV fluids: To correct fluid and electrolyte imbalance and dehydration, IV fluids are administered prior to surgery.
- Antibiotic therapy: To prevent sepsis, antibiotics are administered until surgery is performed.
- Drainage: When perforation of the appendix occurs, an abscess may form and patient is initially treated with antibiotics and the surgeon may place a drain in the abscess.
Surgical Management
Immediate surgery is typically indicated if appendicitis is diagnosed.
- Appendectomy. Appendectomy or the surgical removal of the appendix is performed as soon as it is possible to decrease the risk of perforation.
- Laparotomy and laparoscopy. Both of these procedures are safe and effective in the treatment of appendicitis with perforation.
Nursing Management
- A focus of the nurses’ management is the preparation of the patient for surgery.
Nursing Assessment
Assessment of a patient with appendicitis may be both objective and subjective.
- Assess the level of pain.
- Assess relevant laboratory findings.
- Assess patient’s vital signs in preparation for surgery.
Diagnosis
Based on the assessment data, the most appropriate diagnoses for a patient with appendicitis are:
- Acute pain related to obstructed appendix.
- Risk for deficient fluid volume related to preoperative vomiting, postoperative restrictions.
- Risk for infection related to ruptured appendix.
- Planning & Goals
- Main Article: 4 Appendectomy Nursing Care Plans
Goals for a patient with appendicitis include:
- Relieving pain.
- Preventing fluid volume deficit.
- Reducing anxiety.
- Eliminating infection due to the potential or actual disruption of the GI tract.
- Maintaining skin integrity.
- Attaining optimal nutrition.
Nursing Interventions
- The nurse prepares the patient for surgery.
- IV infusion. An IV infusion is made to replace fluid loss and promote adequate renal functioning.
- Antibiotic therapy. Antibiotic therapy is given to prevent infection.
- Positioning. After the surgery, the nurse places the patient on a High-fowler’s position to reduce the tension on the incision and abdominal organs, thereby reducing pain.
- Oral fluids. When tolerated, oral fluids could be administered.
Evaluation
- Relieved pain.
- Prevented fluid volume deficit.
- Reduced anxiety.
- Eliminated infection due to the potential or actual disruption of the GI tract.
- Maintained skin integrity.
- Attained optimal nutrition.
Discharge and Home Care Guidelines
Discharge teaching for patient and family is imperative.
- Removal of sutures. The nurse instructs the patient to make an appointment with the surgeon to remove the sutures between the 5th and 7th days after surgery.
- Activities. Heavy lifting is to be avoided postoperatively; however, normal activity can be resumed within 2 to 4 weeks.
- Home care. A home care nurse may be needed to assist with incision care and to monitor the patient for complications and wound healing.
Documentation Guidelines
The focus of documentation in patients with appendicitis should include:
- Client’s description of response to pain.
- Acceptable level of pain.
- Prior medication use.
- Results of laboratory tests.
- Surgical site.
- Signs and symptoms of infectious process.
- Recent or current antibiotic therapy.
- Plan of care.
Teaching plan.
- Response to interventions, teaching, and actions performed.
- Attainment or progress toward desired outcomes.
- Modifications to plan of care.
Long term needs.
Nursing Intervention
Preoperative interventions
- Maintain NPO status.
- Administer fluids intravenously to prevent dehydration.
- Monitor for changes in level of pain.
- Monitor for signs of ruptured appendix and peritonitis
- Position right-side lying or low to semi fowler position to promote comfort.
- Monitor bowel sounds.
- Apply ice packs to abdomen every hour for 20-30 minutes as prescribed.
- Administer antibiotics as prescribed
- Avoid the application of heat in the abdomen.
- Avoid laxatives or enema.
Postoperative interventions
- Monitor temperature for signs of infection.
- Assess incision for signs of infection such as redness, swelling and pain.
- Maintain NPO status until bowel function has returned.
- Advance diet gradually or as tolerated or as prescribed when bowel sound return.
- If ruptured of appendix occurred, expect a Penros drain to be inserted, or the incision maybe left to heal inside out.
- Expect that drainage from the Penros drain maybe profuse for the first 2 hours.
Frequently Asked Questions
1. How Do You Rule Out Appendicitis?
- Appendicitis can be ruled out by using brief case history, physical examinations, computed tomography scan, urine analysis, ultrasound abdomen, anal examinations, an x-ray of the abdomen, and blood examination.
2. How Long Can You Have Appendicitis Before It Bursts?
- The duration taken for bursting depends on the type of appendicitis. In the case of chronic appendicitis, it lasts for a long period, whereas in the case of acute conditions, symptoms will appear suddenly and immediate surgery is needed.
3. What Does Appendicitis Feel Like?
- Appendicitis pain might be mild or severe. There will be fever, abdominal pain, navel pain, difficulty in moving around, loss of appetite, and anal pain in some cases. There may also be vomiting, diarrhea, and nausea.
4. How Bad Is Appendicitis Pain?
- There will be sharp pricking pain in the abdomen and the pain worsens by pressing the painful area, moving around. Sometimes, even coughing, and sneezing worsens the pain. There will be difficulty in sitting in a particular place for a long time. There will also be difficulty in passing urine.
5. How Do You Check for Appendicitis at Home?
- There are no standard methods for the examination of appendicitis at home, but we can check for any swelling in the abdominal area. If we have basic knowledge and ideas about appendicitis we can palpate the abdomen and rule out in some cases.
6. How Does Someone Get Appendicitis?
- Any blockages in the lining of the appendix lead to appendicitis. This is mainly due to the food items we consume and seeds of fruits that block the passage. It may lead to infection and rupture in the appendix region and sometimes pus discharges also.
7. Should You Feel for Appendicitis?
- Appendicitis treated at an early time is easily curable but in cases where it is left untreated leads to fatal conditions. So, it is necessary to start the treatment faster. This will make the condition simple.
8. How Does Appendicitis Pain Start?
- The pain usually comes and goes for a short period of time in the belly and navel region. It starts with pain around the navel region which makes it difficult in sitting and moving. If you are feeling too much pain, you should consult your doctor immediately.
9. What Is the Recovery Time for Appendicitis?
- Usually, it takes around one to three days for recovery for laparoscopy. It usually takes two to four weeks after surgery to return to our routine life. Depending on the severity of the surgery, and the patient the recovery time may be extended. You should ask your doctor for instructions that are to be followed.
10. How Quickly Does Appendicitis Come On?
- Appendicitis comes so quickly that symptoms appear within the first 24 hours. Later on, any disturbance and food items lead to further signs and rupture. Any disturbance to the regions leads to further signs.
11. How Long Are a Patient Stays in the Hospital for Appendicitis?
- The patient stays in the hospital just for three days. The patient is admitted to the hospital one day before the surgery. This is done so that the patient can adapt to the environment before the surgery. The next day surgery is performed. The patient is asked to stay in the hospital for another day and then they can be discharged if the doctor advises them to do so.
12. How Quickly Does Appendicitis Develop?
- The degree of pain and the duration it takes to show the symptoms might vary. Appendicitis usually develops in teenagers, the symptoms appear very early in addition some food items lead to rupture of the appendix. Symptoms and signs appear in an early stage. However, you should consult your doctor if you experience pain for more than one day.
13. Where Does Your Stomach Hurt With Appendicitis?
- Initially, the pain starts near the belly and in the navel region, and later on the pain travels to the abdominal region, mainly to the right abdomen. There will be swelling in the stomach region which can be identified by palpation by the doctors. Palpation is the procedure of investigation done by touching and pressing.
14. What Is Appendicitis Surgery?
- For severe cases of appendicitis, appendectomy is done. It is the surgical removal of the appendix. This is usually done by open surgery. Nowadays, it is done using a laser. The surgery that is done using a laser is known as laparoscopy. In which three holes are made and the further procedure is carried out.
15. What Foods Make Appendicitis Worse?
- Undigested food makes the condition of the appendix to worsen. Seeds of fruits and vegetables are also harmful. Medications that are taken to relieve pain leads to the rupture of the appendix. This makes the condition even worsen. Some doctors say that spicy food items also worsen the condition of appendicitis.
16. What are the early signs and symptoms of appendicitis?
The signs and symptoms of appendicitis are:
– Nausea.
– Vomiting.
– Loss of appetite.
– Sudden and severe pain in the right side of the lower abdomen.
– The pain begins in the navel that shifts to the right side of the abdomen.
– Severe pain will be experienced while walking, coughing, and movements.
References:
https://nurseslabs.com/appendicitis/
https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/appendectomy
https://www.healthline.com/health/appendicitis#tests
https://www.icliniq.com/articles/gastro-health/appendicitis
https://teachmepaediatrics.com/surgery/abdominal/acute-appendicitis/

Only wanna remark that you have a very decent web site , I enjoy the design and style it really stands out. Diena Des Maure
Hello! This is kind of off topic but I need some guidance from an established blog. Melli Ettore Coit
Hi there colleagues, good article and nice urging commented here, I am actually enjoying by these. Mindy Ezekiel Griffy
I really enjoy the article. Much thanks again. Will read on… Eadith Ab Pollyanna
This is one awesome article.Really looking forward to read more. Much obliged. Terina Seiber
Awesome article post. Much obliged. Sherwood Bowes