1. A fracture is a break in the continuity of the bone.
2. Common fracture sites:
- Clavicle
- Humerus – In subpracondylar fractures, which occur when child falls backward on hands
 with elbows straight, there is a high incidence of neurovascular complications due to the anatomic relationship of the brachial artery and nerves to the fracture site.
with elbows straight, there is a high incidence of neurovascular complications due to the anatomic relationship of the brachial artery and nerves to the fracture site. - Radius and ulna
- Femur (often associated with child abuse)
- Epiphyseal plates (potential for growth deformity)
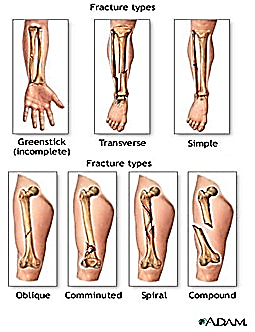
3. Types of Fracture
- Closed or simple fracture – The bone is broken, but the skin is not lacerated.
- Open or compound fracture – The skin may be pierced by the bone or by a blow that breaks the skin at the time of the fracture. The bone may or may not be visible in the wound.
- Transverse fracture – The fracture is at right angles to the long axis of the bone.
- Greenstick fracture – Fracture on one side of the bone, causing a bend on the other side of the bone.
- Comminuted fracture – A fracture that results in three or more bone fragments.
- Oblique Fracture – The fracture is diagonal to a bone’s long axis.
- Spiral Fracture – At least one part of the bone has been twisted.
4. Complications of fracture include:
- problems associated with immobility (muscle atrophy, joint contracture, pressure sores)
- growth problems ( in children)
- infection
- shock
- venous stasis and thromboembolism
- pulmonary emboli and fat emboli
- and bone union problems
B. Etiology
- Fracture in children usually are the result of trauma from motor vehicle accidents, falls or child abuse.
- Because of the resilience of the soft tissue of children, fracture occur more often than soft tissue injuries.
C. Pathopysiology
- Fractures occur when the resistance of bone against the stress being exerted yields to the stress force.
- Fractures most commonly seen in children:
- Bend Fracture – is characterized by the bone bending to the breaking point and not straightening without intervention.
- Buckle fracture – results from compression failure of the bone, with the bone telescoping on itself.
- Greenstick fracture – is an incomplete fracture.
D. Assessment Findings
1. Clinical Manifestations
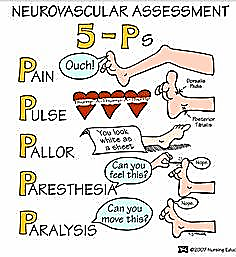
- The five “Ps” – pain, pulse, pallor, paresthesia, and paralysis are seen with all types of fractures.
 Other characteristic findings include deformity, swelling, bruising, muscle spasms, tenderness, pain, impaired sensation, loss of function, abnormality, crepitus, shock or refusal to walk (in small children).
Other characteristic findings include deformity, swelling, bruising, muscle spasms, tenderness, pain, impaired sensation, loss of function, abnormality, crepitus, shock or refusal to walk (in small children).- Laboratory and diagnostic findings
- Radiographic examination reveals initial injury and subsequent healing progress. A comparison film of an opposite, unaffected extremity is often used to look for subtle changes in the affected extremity.
- Blood studies reveal bleeding (decreased hemoglobin and hematocrit) and muscle damage (elevated aspartate transaminase (AST) and lactic dehygrogenase (LHD).
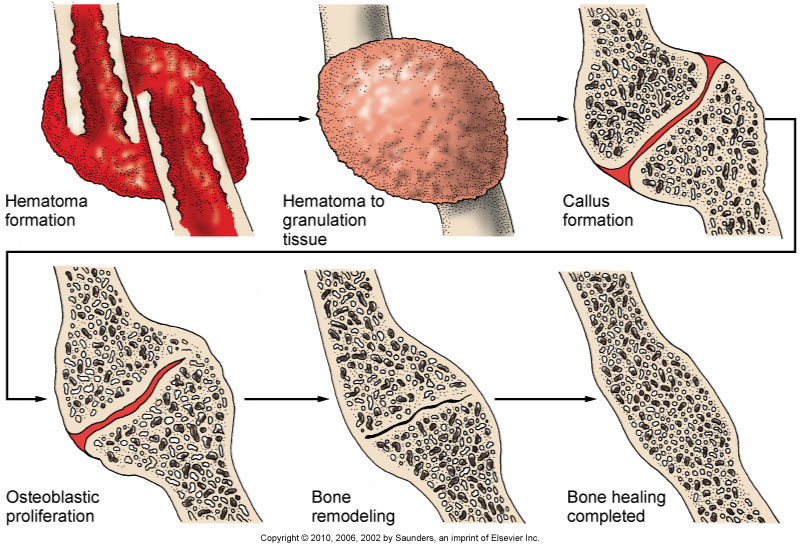
Fracture Healing
Reparative process of self-healing (union) occurs in the following stages:
- Fracture hematoma (d/t bleeding, edema)
- Granulation tissue → osteoid (3 – 14 days post injury)
- Callus formation (minerals deposited in osteoid)
- Ossification (3 wks – 6 mos)
- Consolidation (distance between fragments decreases → closes).
- Remodeling (union completed; remodels to original shape, strength)
COMPLICATIONS OF FRACTURES
- Shock
- With severe injuries or femur fracture
- Neurogenic
- Hypovolemic
- Due to loss of blood volume
- Nursing Action: Replace BV, Relieve Pain, Adequate splinting/mobilization
- With severe injuries or femur fracture
- Fat Embolism Syndrome
- Occurs within 24-72 hours and can also occur up to 1 week after injury
- Seen more severe injuries
- Mostly men 20-30 y/o
- FIRST Symptom: Change in Mental status (mild agitation – Confusion – Delirium – Coma)
- Tachycardia, SOB, Dyspnea, tachypnea, petechia on shoulder and conjunctiva
- First give increased concentration of O2
- Steroids
- Occurs within 24-72 hours and can also occur up to 1 week after injury
- Compartment Syndrome
- Swelling peaks at 24-48 hours after fracture
- Signs and Symptoms
- Deep Throbbing pain that doesn’t respond to morphine
- Muscle is hard
- Diminished capillary refill
- Cyanotic nail beds
- Paralysis
- Parasthsia
- Edema – Can’t get a pulse
- Other Complications
- Thromboembolism
- Infection
- DIC – Disseminated Intravascular Coagulation
- Delayed Complications
- Delayed Union
- Healing not at rate expected possible due to Steroids, diabetic, age
- Non Union
- Bone didn’t unite the way is should
- Avascular Necrosis
- Complete blood loss to bone or neck of femur
- Reaction to Internal Fixation Devices
- Left in permanently – a rare occurrence
- Treatment is by removal of hardware
- Osteomyelitis
- Infection of bone occur with our without surgery
- Delayed Union
- Emergency: Maintain airway, assess distal pulses
E. Nursing Management
- Provide emergency management when situation warrants, for a new fracture.
- Assess the five “Ps”.
- Determine the mechanism of injury.
- Immobilize the part. Move injured parts as little as possible.
- Cover any open wounds with a sterile, or clean dressing.
- Reassess the five “Ps”.
- Apply traction if circulatory compromise is present.
- Elevate the injured limb, if possible.
- Apply cold to the injured area.
- Call emergency medical services.
- Assess for circulatory impairment (cyanosis, coldness, mottling, decreased peripheral pulses, positive blanch sign, edema not relieved by elevation, pain or cramping).
- Assess for neurologic impairment (lack of sensation or movement, pain, or tenderness, or numbness and tingling).
- Administer analgesic medications.
- Explain fracture management to the child and family. Depending on the type of break and its location, repair (by realignment or reduction) may be made by closed or open reduction followed by immobilization with a splint, traction or a cast.
- Maintain skin integrity and prevent breakdown. Institute appropriate measures for cast and appliance care.
- Prevent Complications
- Prevent circulatory impairment by assessing pulses, color and temperature, and by reporting changes immediately.
- Prevent nerve compression syndromes by testing sensation and motor function, including subjective symptoms of pain, muscular weakness, burning sensation, limited ROM, and altered sensation. Correct alignment to alleviate pressure if appropriate, and notify the health care provider.
- Prevent compartment syndrome by assessing for muscle weakness and pain out of proportion to injury. Early detection is critical to prevent tissue damage.
- Causes of compartment syndrome include tight dressings or casts, hemorrhage, trauma, burns and surgery.
- Treatment entails pressure relief, which sometimes require performing a fasciotomy.
- Prevent infection, including osteomyelitits, bys using infection control measures.
- Prevent renal calculi by encouraging fluids, monitoring I&O, and mobilizing the child as much as possible.
- Prevent pulmonary emboli by carefully monitoring adolescents and children with multiple fractures. Emboli generally occur within the first 24 hours.
