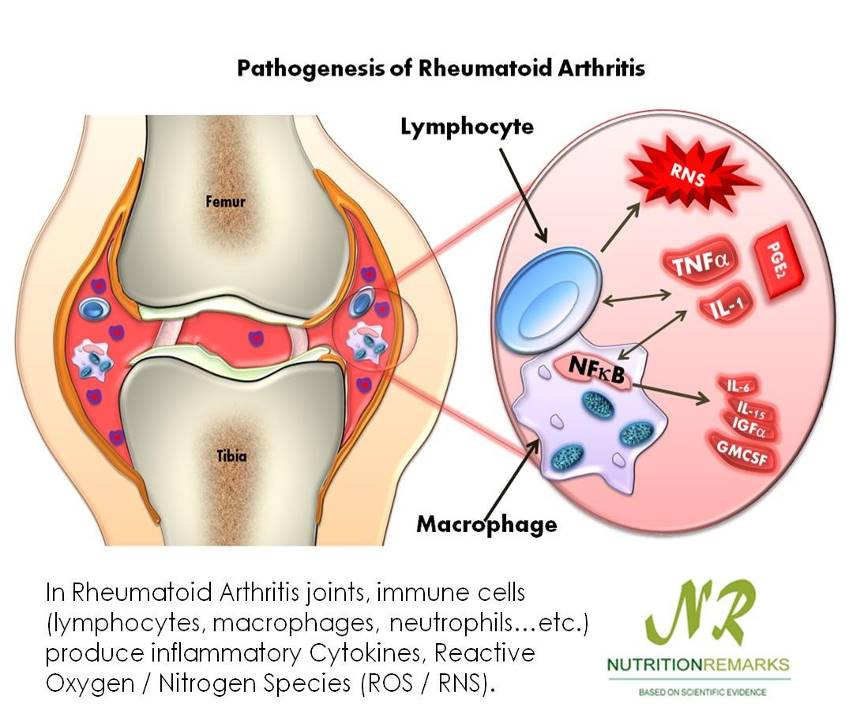
Rheumatoid arthritis is a chronic, systemic autoimmune disease that affects all areas of the body; inflammatory responses occur in all connective tissue. Early symptoms include inflammation of the synovial joints.
- Joint involvement progresses in stages; if disease is diagnosed early, permanent joint deterioration may be prevented.
 The synovium becomes thickened and inflamed, and fluid accumulates in the joint space; this causes a pannus to form.
The synovium becomes thickened and inflamed, and fluid accumulates in the joint space; this causes a pannus to form.- The pannus tissue erodes the cartilage and destroys the joint.
- In medicine, pannus is any abnormal tissue that: Contains blood vessels.
- Type of chronic systemic inflammatory arthritis and connective tissue disorder affecting more women (ages 35-45) than men—3:1.
FACTORS
- Genetic
- Autoimmune connective tissue disorders
- Fatigue, emotional stress, cold, infection
ASSESSMENT FINDINGS
- Joint involvement is symmetrical and bilateral.
- Characteristically beginning in the hands, wrist and feet.
- Joint stiffness occurs early morning, lasts more than 30 minutes, not relieved by movement, and diminishes as the day progresses.
- Joints are swollen and warm.
 Painful when moved.
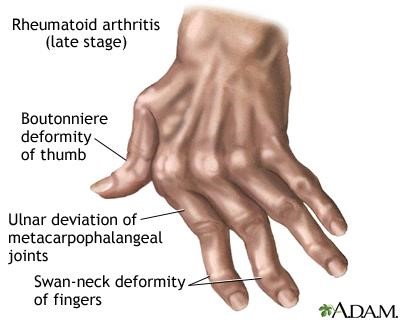
Painful when moved.- Deformities are common in the hands and feet causing misalignment.
- Rheumatoid nodules may be found in the subcutaneous tissues.
DIAGNOSTIC TESTS
- X-ray shows a marked deformity.
- Blood studies reveal (+) elevated ESR and CRP. ***also ANA and RF
- Arthrocentesis shows synovial fluid that is cloudy, milky or dark yellow containing numerous WBC and inflammatory proteins.
MEDICAL MANAGEMENT
- Therapeutic dose of NSAIDS and Aspirin to reduce inflammation.
- Chemotherapy with methotrexate and gold therapy.
- IM or oral preparation
- Takes several months (3-6) before effects can be seen.
- May cause bone marrow depression.
NURSING MANAGEMENT
- Relieve pain and discomfort.
- Use splints to immobilize the affected extremity during acute stage of the disease and inflammation to reduce deformity.
- Suggest application of COLD PACKS during the acute phase of pain, and then HEAT application as the inflammation subsides.
- Decrease patient’s fatigue.
- Scheduled activity when pain is less severe.
- Provide adequate periods of rests.
- Promote restorative sleep.
- Increase patient mobility.
- Advise proper posture and body mechanics.
- Support joint in functional position.
- Advise active ROM.
- Provide diet therapy.
- Patients experience anorexia, nausea and weight loss
- Gluten free diet
- Oats, wheat, cucumber
- Supplements of vitamins, iron and protein
| Definition | Gouty Arthritis | Rheumatoid Arthritis | Osteoarthritis |
| Definition | Uric acid build up in blood and causes joint swelling and pain | Inflammation of joints and surrounding tissue | Due to aging, wear and tear on a joint |
| Population | Male | Female | Both |
| Etiology | Metabolic | Autoimmune | Degenerative |
| Affected | Lower extremities | Upper extremities | Weight bearing joints |
| Hallmark Sign | Tophi | Mirror Image Ankylosis | Heberden’s Nodes
Bouchards Crepitus |
Heberden’s nodes are hard or bony swellings that can develop in the distal interphalangeal joints (DIP) (the joints closest to the end of the fingers and toes). They are a sign of osteoarthritis and are caused by formation of osteophytes (calcific spurs) of the articular (joint) cartilage in response to repeated trauma at the joint.
Bouchard’s nodes are hard, bony outgrowths or gelatinous cysts on the proximal interphalangeal joints (the middle joints of fingers or toes.) They are seen in osteoarthritis, where they are caused by formation of calcific spurs of the articular (joint) cartilage.
Crepitus (also termed crepitation) is a medical term to describe the grating, crackling or popping sounds and sensations experienced under the skin and joints or a crackling sensation due to the presence of air in the subcutaneous tissue.
