Multiple sclerosis (MS) is a chronic demyelinating disease that affects the myelin sheath of neurons in the CNS.
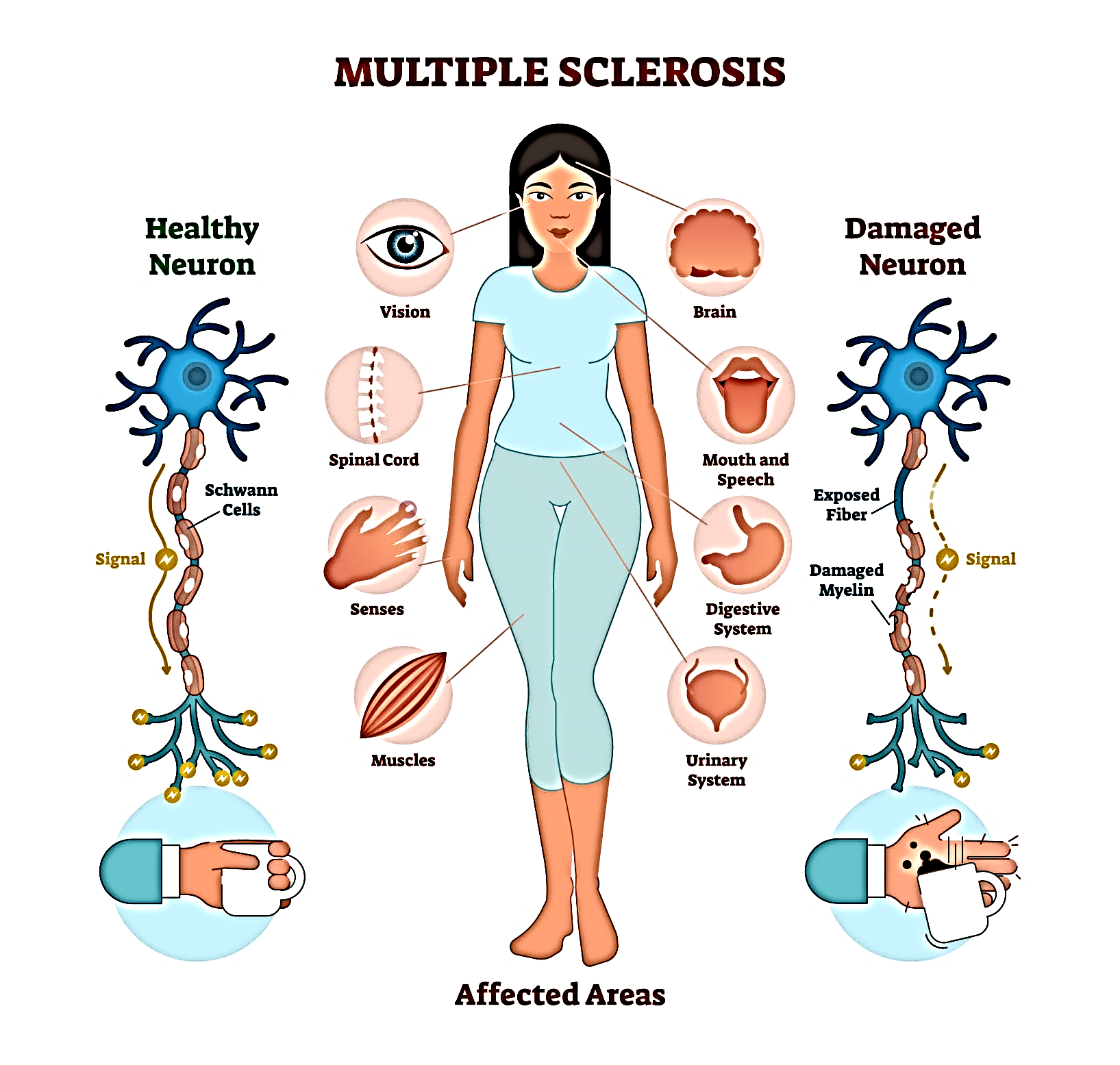 Multiple sclerosis is a disease that causes vision problems, numbness and tingling, muscle weakness, and other problems. It happens when the body’s infection-fighting system attacks and damages nerve cells and their connections in the brain and spinal cord.
Multiple sclerosis is a disease that causes vision problems, numbness and tingling, muscle weakness, and other problems. It happens when the body’s infection-fighting system attacks and damages nerve cells and their connections in the brain and spinal cord.
When the body’s infection-fighting system, called the “immune system,” attacks the body’s own cells, it is called an “autoimmune response.” It causes damage to myelin, the protective coating around the nerves. When myelin is damaged, messages can no longer be clearly transmitted from the brain and spinal cord to other parts of the body. Many people refer to multiple sclerosis as “MS.”
INCIDENCE
- Onset occurs between 20-40 years of age.
- Women are more affected than men. (AANN, 2011).
- Whites are more affected than Hispanics, blacks, or Asians.
- Most prevalent in colder climates of North America & Europe.
- Migration.
ETIOLOGY & RISK FACTORS
- Exact cause is not known yet.
- Most theories suggest that MS is an immunogenetic viral disease (with Epstein Barr virus).
Risk factors are:
- Age (most of the time between 20-40 yrs).
- Sex (women have more chance).
- Family history (genetic susceptibility).
- Certain infections (like Epsteinbarr virus).
- Climate (more in cold climate areas).
- Certain auto-immune diseases (higher risks with thyroid disease, type-1 DM or IBD).
- Smoking.
- Stress, fatigue.
- Physical injury.
- Pregnancy (may relating to stress to labour, or puerperium).
PATHOPHYSIOLOGY
Due to etiological factors
Activated T-cells (which recognise self Ag) expressed in CNS, &
Macrophages (B-cells) enters the brain from peripherral circulation
Production of inflammatory cytokines & reactive O2 species
Inflammation
Then activated T-cells & B-cells cause demyelination and destruction of oligodendrocytes
Formation of plaque Causes scarring & destruction of sheath
Compensatory system starts causing subsidation of edema & inflammation
After that some remyelination process occurs which is often incomplete Multiple sclerosis.
CLINICAL MANIFESTATIONS
The course of illness varies from person to person.
- Fatigue is the lack of physical and mental energy that impacts daily tasks. Fatigue can be physical or mental and is not correlated to how much rest or sleep a person gets. It is one of the most common symptoms and impacts about 80 percent of people living with MS. It can be
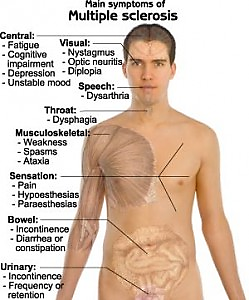 the most debilitating factor, even for those who have minimal physical restrictions, and is one of the leading causes for people leaving the workforce.
the most debilitating factor, even for those who have minimal physical restrictions, and is one of the leading causes for people leaving the workforce. - Heat intolerance in MS is a temporary worsening of symptoms with elevated body temperatures including hot and humid weather, exercising, sunbathing, or fevers. A small rise in body temperature (a quarter to a half a degree) can cause increased fatigue, tingling, blurry vision, or even the inability to walk. Most people living with MS have to avoid outdoor activity and/or use cooling garments to complete simple, daily activities due to this intolerance.
- Cognitive dysfunction affects high-level brain functions such as memory, attention/concentration, the ability to solve daily problems, understand and use language, and process information from different senses. Impaired cognition affects 50-65 percent of those living with MS and is another major reason for leaving the workforce early.
- Pain/abnormal sensation is a common symptom with MS and can be directly related to neuropathic pain (the disease process itself) or from musculoskeletal pain (changes to the body and immobility). The pain experience is unique to each person and can greatly limit his or her ability to participate in and enjoy socialization and activities. Those living with MS can also experience various abnormal sensations such as numbness and tingling, prickling, sharp/stabbing pains, hot/cold sensations, and burning pains which can also impact movement and daily function.
- Depression comes in various forms and can be one of the most common symptoms in MS, more common in people with MS than the general population. Depression can happen to anyone at any time during the disease course and does not correlate to disease severity, however it can greatly impact someone’s quality of life and ability to participate in daily activities.
COMPLICATIONS
People with multiple sclerosis may also develop:
- Muscle stiffness or spasms
- Paralysis, typically in the legs
- Problems with bladder, bowel or sexual function
- Mental changes, such as forgetfulness or mood swings
- Depression
- Epilepsy
DIAGNOSTIC EVALUATION
- There is no definitive test for MS.
- Detailed history of episodes of neurologic dysfunction
- Physical examination.
Other tests include:-
- CSF evaluation (for presence of IgG antibody or oligoclonal bonding)
- Evoked potentials of optic pathways & auditory system to assess presence of slowed nerve conduction.
- MRI of brain and spinal cord (to determine the presence of MS plaques)
- CT scan (to detect areas of demyelination, but with less detail as by MRI).
MEDICAL MANAGEMENT
• No exact cure.
• Aim is to prevent or postpone the long term disability (often evolves slowly over many years).
• The treatment falls into 3 categories:-
1. Treatment of acute relapses.
2. Treatment aimed at disease management.
3. Symptomatic treatment.
1. Treatment of acute relapse:-
- Corticosteroid therapy ( anti-inflammatory & immunosuppressive property )
- For example:
- Methyl-prednisolone , (given I.V. or orally)
- Azathioprine & cyclophosphamide (in severe cases)
2. Treat exacerbations:- (treatment aimed at disease management)
- Interferon-Beta 1b
- Betaseron, given subcutaneously. (antiviral & immuno-regulatory) (For ambulatory clients with relapsing –remitting).
- Interferon Beta 1a
- Avonex, (for treating replasing form of MS).
- Glatiramer acetate
- Copaxane, (for relapsing re-emitting MS).
3. Symptomatic treatment:-
- For bladder dysfunction:
- oxybutynin, propantheline.
- For constipation:
- psyllium hydrophilic mucilloid, suppositories.
- For fatigue:
- amantadine, modafinil .
- For spasticity:
- baclofen, diazefen, dantrolone.
- For Tremor :
- propanolol, phenobarbital, clonazepam.
- For dysesthesias & trigeminal neurolgia:
- carbamazepine, phenytoin, amitriptyline.
- For dysesthesias:
- Transcutaneous electrical nerve stimulation (TENS) is also helpful.
4. Nutritional therapy:-
- Megavitamin therapy (cobalamin/vit. B12 and vit. C)
- Low fat diet.
- high roughage diet (to relieve constipation)
5. Other therapies:- (to improve neurological functioning)
- Physical and speech therapies.
- Exercise.
- Water exercise.
SURGICAL MANAGEMENT
- Deep brain stimulation:-
- if other options have failed then a device is implanted that stimulates an area of brain. (in case of severe tremor in limbs).
- Implantation of a drug catheter or pump:
- a catheter is placed in lower spinal area to deliver a constant flow of drug like baclofen. (in case of severe pain or spasticity).
NURSING DIAGNOSIS:
-
- Impaired physical mobility related to fatigue & weakness
- Activity intolerance r/t weakness, dizziness, and unsteady gait
- Self-esteem disturbance r/t loss of health & lifestyle changes
NURSING MANAGEMENT
-
- Promotes physical mobility – activity and rest
- no vigorous physical exercise
- frequent rest periods
- walking and gait exercises
- minimize spasticity and contractures – warm packs, daily muscle stretching
- activities: swimming, stationary bike, progressive wt bearing
- Minimize effects of immobility; skin integrity; cough and deep breathing exercises.
- Prevent injury – walk with feet wide apart, environment awareness and modification, gait training. Use of assistive devices – walker, cane etc.
- Promote bladder & bowel control – Urinal/bedpan readily available, po fluids intake schedule/voiding schedule, increase fiber in diet, intermittent self-catheterization
- Improve sensory and cognitive function:
- Vision – eye patch for diplopia; prism glasses for reading; talking books
- Speech – slurred, low volume, problems with phonation – speech therapist
- Cognitive & emotional responses – forgetfulness, easily distracted, emotionally labile, social activities; hobbies.
- Development of coping strengths – education about diseases process; stress relief; network of services – social, speech, PT, psychological, homemaker/meal on wheels
- Improve self-care – assistive devices, raised toilet seat, shower bench, reached tongs, decrease physical and emotional stress, decrease exposure of extreme temperatures
- Adapting to sexual dysfunction – counseling, plan sexual activity, willingness to experiment.
