What is monkeypox?
What is monkeypox?
The monkeypox virus causes the disease monkeypox. It is a zoonotic viral illness, which means it may pass from animals to people. It may also transmit from humans to humans and from people to the environment.
What are the symptoms of monkeypox?
Monkeypox can produce a variety of symptoms. While some individuals experience milder symptoms, others may develop more serious illnesses and need hospitalisation. Pregnant women, children, and anyone with impaired immune systems are at a greater risk.
During the 2022 epidemic, the most frequent symptoms of monkeypox were fever, headache, muscular pains, back pain, poor energy, and enlarged lymph nodes, followed or accompanied by the formation of a rash that might last two to three weeks. The rash might appear on the face, palms of hands, soles of feet, groyne, genital, and/or anal areas. It may also be discovered in the mouth, throat, anus, or vagina, as well as on the eyes. The number of sores might vary between one and thousands. Sores on the skin begin flat, then fill with fluids before crusting over, drying up, and falling off, leaving a new layer of skin behind.
There are continuing research to monitor and better understand symptoms during this new epidemic, such as which regions of the body may be impacted and how long symptoms may remain.
Anyone experiencing symptoms of monkeypox or who has had contact with someone who has monkeypox should contact or see a health care practitioner for help.
Symptoms normally resolve on their own or with supportive treatment, such as pain or fever medicine. People are contagious until all lesions have crusted over, scabs have dropped off, and a new layer of skin has developed underneath.
Can people get seriously ill or die from monkeypox?
Most people with monkeypox get better on their own after a few weeks. But for some people, an illness can cause health problems or even death. From what we know about past monkeypox cases, we know that newborn babies, children, and people with weakened immune systems may be more likely to have more severe symptoms or even die from monkeypox.
Monkeypox can lead to complications like secondary skin infections, asthma, confusion, and problems with the eyes. Some newer problems are proctitis, which is painful spots and growth inside the rectum, and pain or trouble peeing. People with monkeypox have died between 1% and 10% of the time in the past. It’s important to remember that death rates can be different in different places because of things like how easy it is to get health care. Because monitoring for monkeypox hasn’t been very good in the past, these numbers may be too high.
Some deaths have been reported in the new countries where the latest outbreak is taking place. This shows how important monkeypox is and how people should keep doing everything they can to protect themselves and others.
How is monkeypox transmitted from person to person?
Close contact with someone who has a monkeypox rash distributes the disease from person to person. Face-to-face contact (such as talking, breathing, or singing close to one another, which can generate droplets or short-range aerosols); skin-to-skin contact (such as touching or vaginal/anal sex); mouth-to-mouth contact (such as kissing); or mouth-to-skin contact (such as oral sex or kissing the skin) are all examples of close contact. The processes of monkeypox transmission via the air are not fully known, and research is being conducted to understand more.
We are still learning how long people with monkeypox are infectious, but they are generally considered infectious until all of their sores have crusted over, the scabs have fallen off and a new layer of skin has formed beneath, and all sores on the eyes and in the body (in the mouth, throat, eyes, vagina, and anus) have healed as well.
When an infected individual touches clothes, bedding, towels, items, devices, or surfaces, the environment might become contaminated with the monkeypox virus. If anybody else touches these goods and has any scrapes or abrasions, or if they accidently contact their eyes, nose, mouth, or other mucous membranes, they may get infected. This is referred to as fomite transmission. Cleaning your hands after contacting potentially infected things may help avoid this form of transfer. Infection may also occur via inhaling skin flakes or viruses from clothes, beds, or towels. Experts are still attempting to figure out if this mechanism of transmission is important in the current epidemic.
The virus may also be transmitted to the foetus during pregnancy, during or after delivery by skin-to-skin contact, or from a parent infected with monkeypox to an infant or kid through intimate contact.
Although asymptomatic infection has been documented, it is unclear if persons who are asymptomatic may transmit the illness or whether the disease can spread via other body fluids. Although a live monkeypox virus has been isolated from sperm, it is unknown if infection may transmit through sperm, vaginal fluids, prenatal fluids, lactation, or blood. More research is being conducted to determine whether or not persons may transmit monkeypox via the sharing of these fluids during and after symptomatic illness.
How is monkeypox transmitted from animals to humans?
Monkeypox can be transmitted to humans through physical contact with an infected animal, such as a non-human primate, terrestrial rodent, antelope, gazelle, or tree squirrel, such as through bites or scratches, or through activities such as hunting, skinning, trapping, cooking, or playing with carcasses. The virus may also be acquired by consuming contaminated animals that have not been completely cooked. Avoiding unprotected contact with wild animals, particularly those that are ill or dead (including their flesh and blood), may lower the chance of contracting monkeypox from them. Any items including animal parts or meat should be fully prepared before consuming in regions where animals spread monkeypox.
Can monkeypox spread from humans to animals?
Monkeypox transmission from people to pets (dogs) is now being explored. Together with our One Health partners, the Food and Agriculture Organisation (FAO) and the World Organisation for Animal Health (WOAH), we are actively watching these developments and considering how to alter our outbreak response and advice if necessary.
Because many animal species are known to be vulnerable to the monkeypox virus, there is the possibility of viral spillover from humans to susceptible animal species in diverse situations, potentially leading to the establishment of new animal reservoirs.
People with monkeypox should avoid close physical contact with animals, including pets (such as cats, dogs, hamsters, gerbils, and so on), livestock, and wildlife.
Who is at risk of catching monkeypox?
People who live with or have close relationships (including sexual contact) with someone infected with monkeypox are the most vulnerable. Anyone who lives with someone who has monkeypox should take precautions to avoid being infected. A person with monkeypox should be evaluated by a health care practitioner to see whether they are healthy enough to be cared for at home and if isolation can be handled safely at home. To protect oneself when caring for monkeypox patients, health staff should practise infection prevention and control methods. Newborn newborns, young children, and persons with underlying immune weaknesses are at a greater risk of developing more severe symptoms, and in rare circumstances, dying from monkeypox. Pregnancy may also raise one’s chances of having a miscarriage or stillbirth.
People who were immunised against smallpox may be immune to monkeypox. Younger individuals, on the other hand, are unlikely to have had smallpox vaccine since the illness was eliminated in most settings worldwide in 1980. People who have received a smallpox vaccination should continue to take steps to protect themselves and others.
What can I do to protect myself and others against monkeypox?
In places where monkeypox is present, avoid unprotected contact with wild animals, particularly those that are ill or dead (including their flesh and blood). Any items containing animal parts or meat should be fully prepared before consumption.
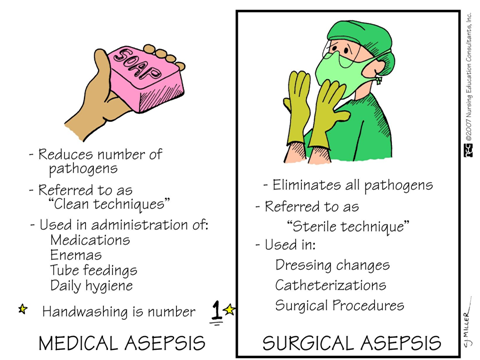
Limit your contact with persons who have suspected or confirmed monkeypox to reduce your chance of contracting it from them. Maintain awareness of monkeypox in your community or social group, and have open dialogues with individuals with whom you have close contact (particularly sexual contact) about any symptoms you or they may be experiencing. Hands should be washed often with soap and water or an alcohol-based hand massage.
Clean and disinfect frequently touched surfaces in locations that might have been contaminated with the virus from an infected person. The monkeypox virus may be killed with common home disinfectants or bleach solutions.
If you suspect you have monkeypox, get medical attention and isolate yourself from others until you have been assessed and tested. If you have monkeypox, you should separate yourself from people until all of your wounds have crusted over, the scabs have come off and a new layer of skin has grown underneath, and all of your internal sores have healed. This will prevent you from spreading the infection to others. Consult your health care provider about whether you should isolate at home or at a health institution. Use condoms as a precaution when having sexual contact for 12 weeks after you have recovered until more is known regarding transmission via sexual fluids.
Can I get monkeypox from touching things and surfaces in public?
Previous monkeypox outbreaks have shown that getting monkeypox after contacting infected materials is possible. If an infected person touches an object, surface, or fabric, it might get contaminated with the monkeypox virus. In some settings, the virus has been discovered to live on various surfaces for some time. However, in this epidemic, researchers are currently investigating whether humans may get monkeypox through contacting surfaces and objects. Currently, practically all instances are connected to close contact, such as touching or intercourse.
To destroy the monkeypox virus, clean objects and surfaces with soap and water, basic home disinfectants, or a bleach product.
What should I do if I have signs of monkeypox or have been around someone who has it?
If you have had close contact with someone who has monkeypox or have been in an area that may have been contaminated with the virus, keep a watchful eye out for signs and symptoms for 21 days following your last exposure. Limit your close contact with other people as much as possible, and let your contacts know if it is unavoidable that you have been exposed to monkeypox.
If you suspect you have monkeypox, contact your healthcare professional for guidance, testing, and medical treatment. Isolate yourself from people as much as possible until you get your test results. Hands should be cleaned on a regular basis.
If you test positive for monkeypox, your doctor will tell you whether you should isolate at home or in a hospital, as well as what kind of treatment you need.
If I have monkeypox, what should I do to protect other people from getting infected?
If you have monkeypox, your doctor will tell you whether you should be treated in a hospital or at home. This will depend on the severity of your symptoms, whether you have risk factors that put you at risk for more severe symptoms, and if you can reduce your chances of infecting everyone you live with.
You should not go out if it is recommended that you isolate at home. Protect those with whom you live as much as possible by:
- Inviting friends and relatives to assist you by providing items you need
- Isolating yourself in a different room
- Having a separate loo or washing after each use
- Using soap and water and a home disinfectant, clean and disinfect regularly touched surfaces.
- Avoid cleaning or vacuuming (this may dislodge virus particles and infect others).
- Before sharing, use separate utensils, items, and devices, or thoroughly clean with soap and water/disinfectant.
- There will be no sharing of towels, beds, or clothing.
- Doing your own laundry (carefully lifting bedding, shirts, and towels without shaking them, placing them in a plastic bag before transporting them to the washing machine, and washing them in hot water > 60 degrees)
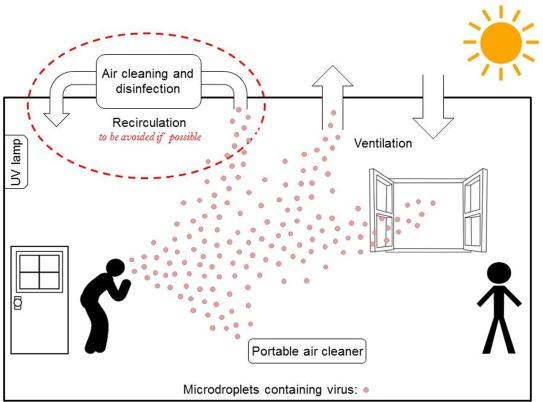
- Ventilation may be improved by opening windows.
- Encourage everyone in the family to wash their hands with soap and water or an alcohol-based hand sanitizer on a frequent basis.
If you can’t avoid being in the same room as someone else or having close contact with another person while isolating yourself at home, try to decrease their danger by:
- Avoiding physical contact
- Hands should be washed often with soap and water or an alcohol-based hand sanitizer.
- Covering your rash with clothes or bandages (until you can isolate again – your rash heals quickest when left alone)
- Leaving windows open around the house
- Ensure that you and everyone else in the room are wearing properly fitted medical masks.
- Keeping at least one metre apart from others
- If you are unable to wash your own laundry and require someone to assist you, they should wear a well-fitting medical mask, disposable gloves, and follow the laundry procedures specified above.
Is there a vaccine against monkeypox?
Yes. There are three vaccinations available to protect against monkeypox. Despite the fact that supplies are now limited, get vaccinated if provided since they provide a vital degree of protection against the illness. After being vaccinated, continue to take precautions to avoid catching and spreading monkeypox; this is because immunity takes several weeks to develop after vaccination, and we don’t yet know how well the vaccines protect you or prevent you from infecting others, as efficacy data in this outbreak setting is needed.
Vaccination is recommended in several nations for those who are at risk. Many years of study have resulted in the creation of improved and safer vaccinations for smallpox, which may also be effective for monkeypox. Two of them (MVA-BN and LC16) have been licenced for monkeypox prophylaxis. Only those who are at risk (for example, someone who has had intimate contact with someone who has monkeypox) should be vaccinated. At this time, mass immunisation is not advised.
While the smallpox vaccination has previously been found to be protective against monkeypox, current evidence on the efficacy of newer smallpox/monkeypox vaccines in the prevention of monkeypox in clinical practise and in field settings is sparse. The study of the usage of monkeypox vaccinations wherever they are used will allow for the quick collection of more information on the efficiency of these vaccines in various circumstances.
How should someone take care of themselves if they have monkeypox? What care do they need?
The care someone need will be determined by their symptoms and their risk of developing a more serious condition. People who have monkeypox should listen to their doctor’s recommendations. Symptoms often last two to three weeks and resolve on their own or with supportive treatment, such as pain or fever medication (such as analgesics and antipyretics).
It is critical for anybody suffering with monkeypox to remain hydrated, eat properly, and get enough sleep. People who are self-isolating should take care of their mental health by doing things they find relaxing and enjoyable, staying connected to loved ones through technology, exercising if they feel well enough and can do so while isolating, and seeking mental health support if necessary.
People suffering from monkeypox should avoid scratching their skin and take care of their rash by washing their hands before and after touching sores and keeping their skin dry and uncovered (unless they are forced to share a room with someone else, in which case they should cover it with clothing or a bandage until they can isolate again). The rash may be cleaned with sterile water or an antiseptic. Saltwater rinses may aid with mouth sores, while warm baths with baking soda and Epsom salts can help with body sores. If necessary, paracetamol may be given to assist control the discomfort produced by sores. A health expert should be consulted if greater pain medication is required.
Many years of study on smallpox therapies have resulted in the discovery of medications that may also be beneficial for treating monkeypox. The European Medicines Agency authorised tecovirimat, an antiviral intended to treat smallpox, for the treatment of monkeypox in exceptional circumstances in January 2022. There has been little experience with these therapies in the setting of a monkeypox epidemic. As a result, their usage is often accompanied by enrollment in a clinical trial or extended access protocol, as well as the gathering of data that will increase understanding on how to effectively utilise them in the future.
Where in the world is there currently a risk of monkeypox?
A multi-country monkeypox epidemic is presently happening throughout Europe, the Americas, Africa, the Western Pacific, Eastern Mediterranean nations, and South East Asia, where the virus has not before been identified. More cases than usual have been documented in 2022 in previously reported areas of Africa, including Nigeria, the Democratic Republic of the Congo, and the Central African Republic. WHO is collaborating with all impacted countries to improve monitoring and give guidelines on how to contain the outbreak and care for patients.
Monkeypox has been documented in various African nations prior to the pandemic. Cameroon, Central African Republic, Republic of the Congo, Côte d’Ivoire, Democratic Republic of the Congo, Gabon, Liberia, Nigeria, and Sierra Leone are among them. Some of these nations experienced just a few instances, while others had continuous or recurring epidemics. Travel from Nigeria has been related to a few instances in other countries. The current epidemic, which is hitting many nations at the same time, is unlike earlier outbreaks.
Is there a risk of this becoming the next pandemic?
Monkeypox is not as infectious as other viruses because it needs intimate contact (e.g., face-to-face, skin-to-skin, mouth-to-skin, or mouth-to-mouth), a contaminated environment, or an infected animal to spread. We have a window of opportunity to stem the spread of this epidemic by collaborating closely with communities and groups at greater risk. It is critical that everyone work together immediately to limit the spread by understanding their risk and taking measures to reduce it. In July, the Director General of WHO declared the monkeypox epidemic a public health emergency of worldwide concern and issued Temporary Recommendations to assist nations in combating and controlling the outbreak.
To prevent future spread, WHO is reacting to this epidemic as a top priority. WHO is focused on learning more about how the virus is spreading during this epidemic and preventing additional individuals from being sick. Raising awareness about this new condition will aid in the prevention of future spread.
What do we know about monkeypox and sex?
Monkeypox may be transmitted by any kind of intimate contact, including kissing, touching, oral and penetrative vaginal or anal intercourse with an infected person. People who have sex with several or new partners are more vulnerable. Although the monkeypox virus has been discovered in sperm, it is still unknown if monkeypox may be transmitted by sperm or vaginal secretions.
If you are having sex, check yourself for symptoms on a frequent basis and advise your partners to do the same. Anyone who develops new or unusual rashes or sores should avoid having sex or other close contact with other people until they have been tested for sexually transmitted diseases (STIs) and monkeypox. Remember that the rash may appear in regions that are difficult to view within the body, such as the mouth, throat, genitals, vagina, and anus/anal area.
Consider decreasing your number of sexual partners to lower your chance of monkeypox. You could wait a while before having sex with new people, or you could stop having sex until the outbreak is under control or until you can get vaccinated (and even then, it’s best to limit your number of partners because no vaccine provides 100% protection and you could still pass the virus on to others). Keep in mind that immunisations take many weeks to work.
If you’re having sex, have open, nonjudgmental talks with your partner or partners and exchange contact information so you may notify each other if you develop symptoms, even if you don’t intend to see each other again.
Wearing a condom will not completely prevent you from monkeypox, but it will minimise your risk or level of exposure and will also protect you and others from a variety of other STIs. People with monkeypox are recommended to wear condoms for 12 weeks following recovery until more is known about virus levels and possible infectivity in sperm during this time.
The virus spreads not just via sexual intercourse, but also through any sort of intimate contact with an infected person. Persons living in the same home are more vulnerable. Anyone experiencing signs of monkeypox should seek medical attention right once.
Are men who have sex with men at higher risk of catching monkeypox?
The danger of monkeypox is not confined to sexually active persons or men who have sex with males. Anyone in close touch with someone suffering from symptoms is at danger. However, the majority of the cases reported in the current epidemic have been detected in males who have intercourse with men. Given that the virus is now spreading from person to person in these social networks, males who have sex with men may be more vulnerable to infection if they have intercourse or other intimate contact with someone who is contagious. People who have several or new sexual partners are the most vulnerable right now.
Monkeypox cases have been detected in sexual health clinics. One reason we’re getting more reports of monkeypox cases among communities of guys who have sex with males is that this demographic group is more health-conscious. Monkeypox rashes may mimic those of sexually transmitted illnesses such as herpes and syphilis, which may explain why these cases are being reported to sexual health clinics. We may find additional examples in the larger community as we learn more. Monkeypox has been discovered in some mothers and children.
Raising awareness among homosexual, bisexual, and other men who have sex with men is critical to protecting those most vulnerable. If you have intercourse with other males, be aware of your risk and take precautions to protect yourself and others. Anyone experiencing symptoms suggestive of monkeypox should seek medical attention promptly to be diagnosed and treated.
What is WHO’s response to stigma and discrimination related to monkeypox?
We’ve witnessed prejudice and messages stigmatising specific categories of individuals in the aftermath of the monkeypox epidemic. We want to make it quite clear that this is not acceptable. This epidemic response should be carried out in accordance with long-standing ideals of human rights, inclusivity, and the dignity of all persons and communities.
Anyone who comes into close personal contact with someone who has monkeypox, regardless of who they are, what they do, who they have sex with, or any other circumstance, is at danger. It is wrong to stigmatise somebody because of a sickness or condition. Stigma is simply going to make things worse and prevent us from stopping this pandemic as soon as possible. We must all work together to support anybody who has been infected or who is assisting in the care of those who are ill. We understand how to halt the spread of this illness and how we can all safeguard ourselves and others. Stigma and prejudice are never acceptable, and they are more so in the context of this epidemic. We’re in this together.
Is my risk of becoming infected, developing serious symptoms or dying from monkeypox higher if I am living with HIV?
Anyone who comes into touch with someone who has monkeypox is at danger of getting it.
HIV may impair your immune system if left untreated. There is some evidence that being immunocompromised may raise your chances of being infected and developing severe disease or dying from monkeypox if you are exposed. More evidence, however, is required to properly comprehend this.
People with preexisting immunological weaknesses may be more vulnerable to monkeypox. People living with HIV who are aware of their status, have access to, and utilise, medication, may achieve viral suppression. This implies that their immune systems are less susceptible to other illnesses than they would be if they were not receiving therapy. Many persons with monkeypox in the present epidemic also had HIV, but there have been very few severe instances of monkeypox, most likely because their HIV infection was well-controlled in the majority of cases. Studies are being conducted to have a better understanding of these issues.
People who have multiple sexual partners, including those living with HIV, are encouraged to take precautions to reduce their risk of exposure to monkeypox by avoiding close contact with anyone who has symptoms and avoiding high-risk situations where multiple contacts may occur, even with people who are unaware they have monkeypox. Having fewer sexual partners may lessen your risk.
Can children get monkeypox?
Children may get monkeypox if they come into touch with someone who is ill. According to data from previously impacted nations, children are more susceptible to serious sickness than adolescents and adults. There have been a few cases of monkeypox among youngsters in the current epidemic. Some children have been exposed to the virus at home via close contact with parents, carers, or other family members. Other children are teens who have had sexual relations with someone infected with monkeypox.
What should I do if a child in my care has symptoms that could be monkeypox?
At first glance, the monkeypox rash resembles other common children diseases such as chickenpox and other viral infections. Consult a healthcare practitioner if a kid you are caring for exhibits signs of monkeypox. They will assist them in getting tested and receiving the necessary treatment.
Children may be more vulnerable to severe monkeypox than adults. They should be constantly watched until they have healed in case they need further treatment. A health professional in charge of the kid may recommend that they be cared for at a health institution. In this case, a healthy parent or carer who is at low risk of monkeypox will be permitted to isolate with them.
What are the risks of monkeypox during pregnancy?
More study is required to better understand the hazards of monkeypox during pregnancy, as well as how the virus may be transmitted to the foetus in the womb, the baby during or after delivery, or during nursing. According to available evidence, acquiring monkeypox during pregnancy may be harmful to the foetus.
Avoid close contact with somebody who has monkeypox if you are pregnant. Anyone who comes into touch with an infected person, regardless of age, may get monkeypox.
Contact your healthcare practitioner if you believe you have been exposed to or are experiencing symptoms of monkeypox. They will assist you in getting tested and receiving the necessary treatment.
Can I continue to breastfeed if I have been diagnosed with monkeypox?
If you have confirmed or suspected monkeypox and are nursing, get guidance from your healthcare professional. They will analyse the danger of spreading monkeypox as well as the risk of depriving your child of nursing. If you can continue to breastfeed and have close contact, they will advise you on how to limit the risk by taking precautions such as covering your sores and wearing a mask to reduce the danger of viral transmission. The danger of infection must be carefully evaluated against the possible damage and suffering caused by discontinuing nursing and close parental-child interaction. It is unknown if the monkeypox virus may be passed from parent to kid via breastfeeding; additional research is needed in this area.
Why is this disease called ‘monkeypox’?
The illness is known as monkeypox because it was discovered in 1958 in study colonies of monkeys. It was only in 1970 that it was discovered in humans. Experts are being consulted on whether the illness should be renamed.
Can the monkeypox virus be spread through a blood transfusion?
You should never give blood if you are sick. If you have a blood donation appointment, examine your health and monitor any signs of monkeypox, and postpone if you don’t feel well.
When individuals may donate blood, severe processes are in place. The potential donor is questioned about their present state of health and any symptoms they are experiencing. This is done to limit the possibility of someone with an infectious illness donating blood.
There have been no cases of monkeypox being transmitted via blood transfusions.
Does past exposure to chickenpox provide any protection against monkeypox?
A separate virus (the varicella virus) causes chickenpox. Past chickenpox exposure does not protect against monkeypox (produced by the monkeypox virus, an orthopoxvirus).
Is there a test to check whether I have had monkeypox in the past?
There are tests available to determine if you have antibodies to orthopoxviruses (the viral family to which monkeypox belongs). These tests may assist determine if you had previously been immunised against smallpox or monkeypox or exposed to an orthopoxvirus. However, the tests cannot tell you if you were exposed to a vaccination, the monkeypox virus, or another orthopoxvirus in the past. As a result, antibody tests are seldom utilised to screen for prior monkeypox exposure or to diagnose a suspected new disease.
I’ve had monkeypox in the past. Can I catch it again?
Our knowledge of how long immunity lasts after monkeypox infection is still limited. We don’t know if a past monkeypox infection provides protection against subsequent infections, and if so, for how long. There have been rare reports of second infections. Even if you have previously had monkeypox, you should take every precaution to prevent being infected again.
If you have had monkeypox in the past and someone in your home now has it, you may protect others by being the designated carer, since you are more likely to be immune than others. You should, however, take all care to prevent being infected.
Are people who are immunosuppressed at higher risk of developing severe mpox?
Immunocompromised patients, notably those with untreated HIV and advanced HIV illness, seem to be at a greater risk of getting severe mpox and dying. Larger, more extensive lesions (particularly in the mouth, eyes, and genitals), secondary bacterial infections of the skin or blood, and lung infections are all symptoms of severe mpox. The statistics reveal that persons with significant immunosuppression (CD4 count fewer than 200 cells/mm3) had the worst symptoms.
People living with HIV who achieve viral suppression by antiretroviral therapy have no increased risk of severe mpox. In the event of infection, effective HIV therapy lowers the likelihood of developing severe mpox symptoms. People who are sexually active and do not know their HIV status should be tested for HIV if it is accessible. HIV-positive people who are receiving effective treatment have the same life expectancy as HIV-negative people. More information may be obtained from your health care provider.
Severe mpox instances in certain countries underscore the critical need to expand equitable access to mpox vaccinations and medicines, as well as HIV prevention, testing, and treatment. Most impacted groups will be left without the tools they need to preserve their sexual health and well-being if this does not happen.
If you have mpox symptoms or believe you may have been exposed, contact your health care provider to get tested for mpox and obtain the information you need to lower your risk of developing more severe symptoms.
 Dengue fever is a mosquito-borne viral infection that can cause flu-like symptoms and, in severe cases, potentially life-threatening complications. It is caused by the dengue virus, which is transmitted to humans primarily through the bite of infected female Aedes mosquitoes, particularly Aedes aegypti and Aedes albopictus. Dengue fever is common in tropical and subtropical regions of the world, including parts of Southeast Asia, the Pacific Islands, the Caribbean, and Central and South America.
Dengue fever is a mosquito-borne viral infection that can cause flu-like symptoms and, in severe cases, potentially life-threatening complications. It is caused by the dengue virus, which is transmitted to humans primarily through the bite of infected female Aedes mosquitoes, particularly Aedes aegypti and Aedes albopictus. Dengue fever is common in tropical and subtropical regions of the world, including parts of Southeast Asia, the Pacific Islands, the Caribbean, and Central and South America.
 What is monkeypox?
What is monkeypox?