- Paget’s disease is a chronic condition of bone characterized by disorder of the normal bone remodeling process.
- Characterized by excessive breakdown of bone tissue followed by abnormal bone formation.
- Also known as Osteitis Deformans is a bone disease unknown cause.
- Affecting men twice as frequently as women.
- Named after the England Surgeons Sir James Paget.
- You’ve probably heard of Paget’s disease, but you may not realize it’s the second most common metabolic bone disease, after osteoporosis. In this chronic and progressive bone-remodeling condition, large and abnormal osteoclasts increase bone resorption (breakdown) at single or multiple bone sites.
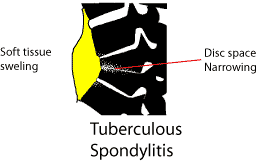
- At first, bone resorption exceeds bone formation. Eventually, normal bone-forming cells (osteoblasts) are stimulated to form new bone rapidly in a disorganized, dysfunctional way. Bones affected by Paget’s disease are larger and weaker than normal, with increased metabolism and blood supply, which in turn can lead to bone pain, arthritis, skeletal deformities, and fractures. Although the disease can affect any bone, the most common sites are the spine, skull, pelvis, and weight-bearing leg bones. Long-term observation indicates that the disease doesn’t spread from one bone to another.
Etiology
- The cause of Paget’s disease is unknown
- Disease may be caused by a virus: Paramyxo virus
- Resulting in localized abnormal osteoclastic activity typical of paget’s disease.
- Also, a person’s genes may predispose them to developing paget’s disease.
- Paget’s disease affects skeletal older bone of adults
- There is also an extremely rare form of paget’s disease in children, referred to as Juvenile Paget’s disease
- In two of every three cases of Paget’s disease, more than one bone is affected
Pathology
- Increased number of osteoclasts. Osteoclasts also often larger. The osteoblasts are normal, but are often over active, due to increased factors released by osteoclasts.
- Essentially, an accelerated rate of bone turnover – with subsequent rapid new bone formation – and this new bone does not have a normal bone matrix – the matrix is disorganised
- The bones increase in size, but become more brittle, and thus more prone to fracture.
Manifestations – Symptoms
- Paget’s disease is more commonly asymptomatic, but may exhibit a variety of non-specific symptoms due to increased bone turnover.
- The bones that are move commonly affected include the pelvis, spine, skull, and the long bone.
- Individuals may experience any or a combination of the following symptoms;
- Bone pain
- fractures
- Pain
- Stiffness
- Difficulty moving your affected joints
- Nerve damage
- Loss of balance
- bone fractures
Other symptoms …
- Hearing loss, Headaches, Osteoarthritis, visual abnormalities, Cardiac abnormalities, Skeletal Deformities
Significant Lab Tests
- Blood chemistry (blood patient who have paget’s disease) results indicate very high alkaline phosphates levels with normal serum calcium and phosphorus.
- Pagetic bone has a characteristic appearance on X-rays.
- ↑level of alkaline phosphatase in the blood.
- Normal calcium, phosphate, & aminotransferase.
- ↑- Markers of bone turnover in urine eg. Deo-pyridinoline
- ↑ – Levels of serum & urinary hydroxyproline.
- Bone scans are useful for extent and activity of the condition.
Imaging Consideration
- X-ray of the skull, spine, pelvis and long bone.
- CT scan
- MRI (Magnetic Resonance Imaging)
- Radionuclide bone scan or RNI (Radionuclide Imaging).
Radiological Appearance
- Radionuclide bone scans readily detect Paget’s disease even in its very early stage.
- Radio graphically of the affected bone typically demonstrate cortical thickening, with a coarse, thickened trabecular pattern.
Complications
- Complications of Paget disease include the following:
- Fractures (abnormal bone)
- Osteogenic Sarcoma
- Neuromuscular syndromes (compression)
- Joint disease (degenerative)
- Cardiovascular abnormalities (hyper-dynamic circulation)
Medical Management
- There is no known cure for this disease.
- Most cases are mild and asymptomatic no treatment is necessary in symptomatic cases medications.
- Bisphosphonates are required to reduce the osteoclastic activity.
- Calcium + Vitamin D + sun shine and Exercies.
- The osteoclastic/osteoblastic activity can be monitored by regular check up of serum/urinary calcium, bone specific alkaline phosphatases.
- Needs management of cardiac problems due to hyper dynamic circulation.
- Watch for Osteogenic sarcomas.
Surgical management
- Deformities may be corrected by surgical intervention (osteotomy). ORIF Open Reduction Internal Fixation may be necessary for fractures.
- Total hip or knee replacement is usually required when client with Paget’s disease develops degenerative arthritis of hip or knee May require surgery for spinal stenosis, nerve root compression
Diet and Exercise
- 1000-1500 mg of Calcium
- Adequate Sunshine
- At least 400 units of Vitamin D DAILY
Teaching Plan
- Patients over the age of 40 can be at risk for Paget’s disease.
- Medical treatment may not cure current health problems associated with Paget’s disease
- Surgery may be needed to reduce pain and increase activity.
- When taking oral medications, patients should drink 6-8 oz of water.
- Patients should remain in an upright position 30 minutes following taking medications.
- Patient should also refrain from eating for 30 minutes following oral medication
- Patients may experience heartburn with oral medications.
- Although the condition is a chronic illness, Paget’s disease focuses on the bones associated with the spine, pelvic, hip, thighs, head and arms but does not spread to new bone.
- Patient needs to adhere to frequent, regular check-ups with treating physicians
- Paget’s disease does not majorly impact the quality of patient life. Research shows many have no critical complaints while living with Paget’s disease.