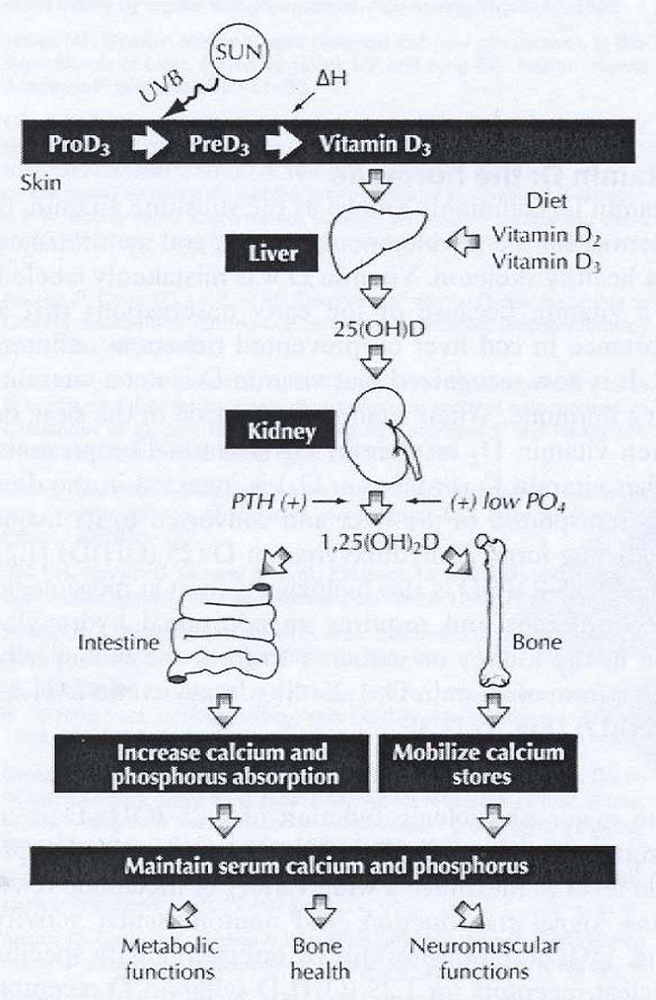
- Decalcification and softening of bones.
- Due to a lack of vitamin D or a problem with the body’s ability to break down and use this vitamin.
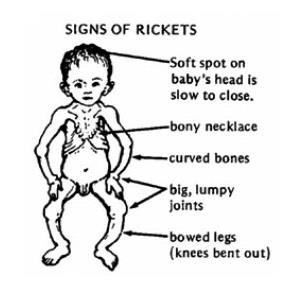
- Rickets in children.
- In adults, the condition is called osteomalacia; and in children, it’s known as rickets. Each one is a condition where prolonged and excessive vitamin D deficiency causes bones to soften, weaken, and easily fracture.
Rickets
- Disease of growing bones of children (in it epiphyseal plate not closed) in which defective mineralization occurs in both bone and cartilage of epiphyseal growth plate.
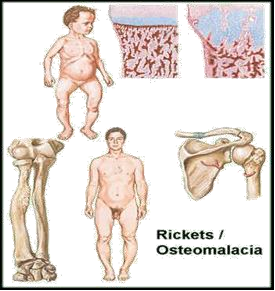 Osteomalacia
Osteomalacia
- Disorder of mature bones in adult (after epiphyseal plate closure) in which mineralization of new osteoid bone is inadequate or delayed
RISK FACTORS
- Chronic diarrhea
- GIT malabsorption
- Lack of exposure to sunlight
- Pregnancy
- Avoidance of milk
- Sedentary lifestyle
- Renal disease
- Use of strong sunscreen
CLINICAL/DIAGNOSTIC MANIFESTATION
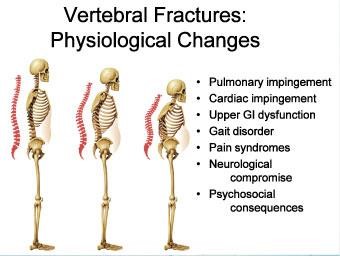
 Fractures
Fractures- Persistent and diffuse skeletal pain
- Progressive deformities of bones
-
- Bowed legs
- Knock knees
- Rachitic rosary
- Enlarged wrists and ankles
- Pigeon breast
-
- Progressive muscle weakness
- Decreased serum levels of Calcium (44-107 IU/L)
- Looser zones on X-ray.
- Roentgenograms shows bone demineralization and multiple bone deformities. (white: more dense; otherwise: black)
- Elevated serum alkaline phosphatase.
NURSING INTERVENTIONS
- Assess posture and gait, note ability to walk with or without aid.
- Note ability to walk requested distances.
- Check bony prominence for pressure sores.
- Assess shapes of bones throughout the body.
- Administer prescribed diet.
- Rich in Calcium
- Rich in Vitamin D (tuna, salmon, mackerel)
- Discuss purpose of physical therapy.
- Assist to a position of comfort.
- Administer prescribed analgesics.
- Gentle back massage.
- Instruct regarding home safety.
- Teach family the effects of Calcium and Vitamin D on the body and the factors affecting absorption.
- Teach client on the signs of fracture.
- Follow up care as needed.
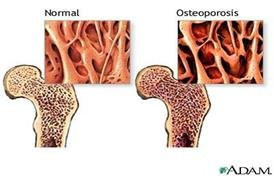
Difference Between Osteoporosis & Osteomalacia
- Osteoporosis refers to the degeneration of already constructed bone, making them brittle,
- While osteomalacia is an abnormality in the building process of bone, making them soft.


 Alcohol overuse
Alcohol overuse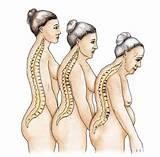
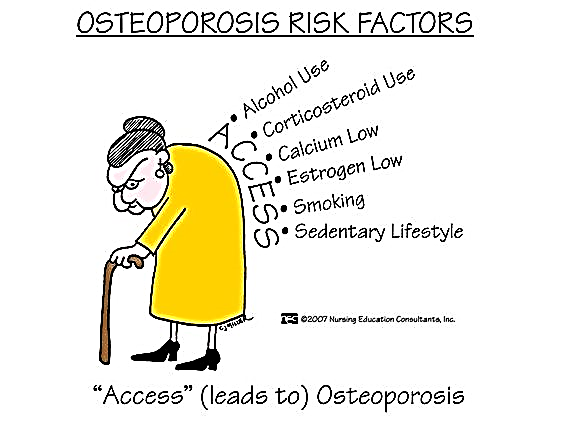 Immobility
Immobility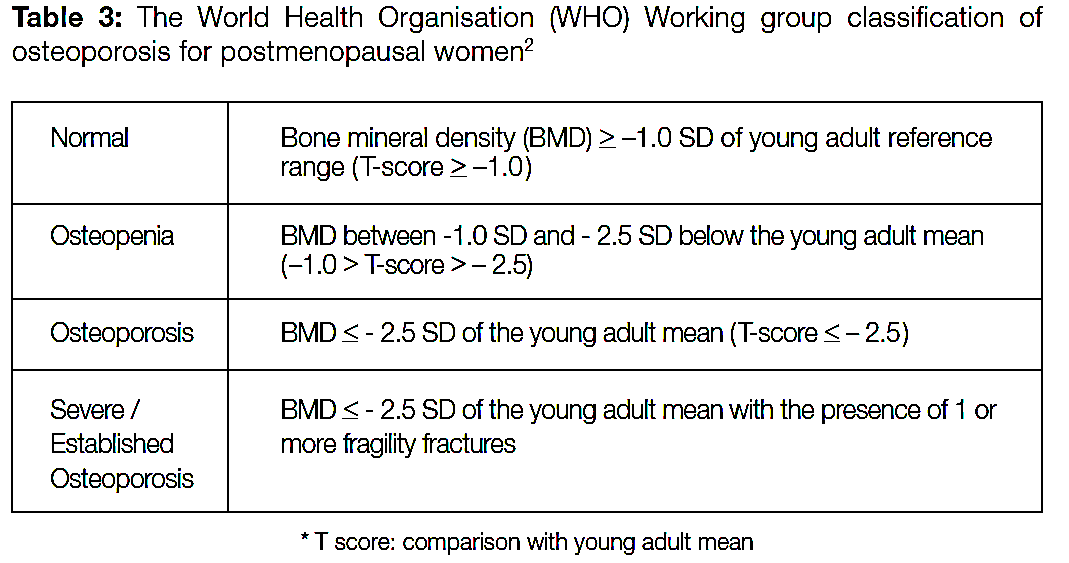 Provide a safe environment.
Provide a safe environment.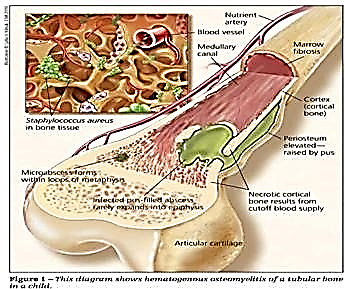 Caused by direct invasion from an open wound or a systemic infection.
Caused by direct invasion from an open wound or a systemic infection.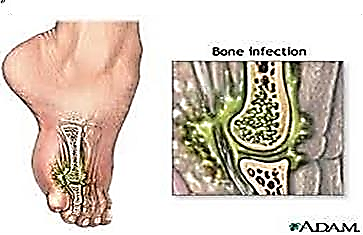
 ETIOLOGIES
ETIOLOGIES  DIAGNOSTIC FINDING
DIAGNOSTIC FINDING 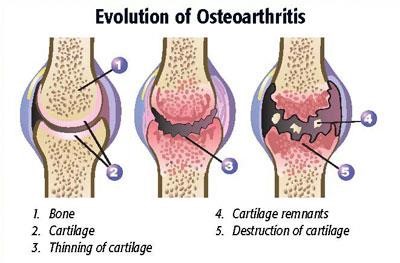 Most common form of degenerative joint disorder.
Most common form of degenerative joint disorder.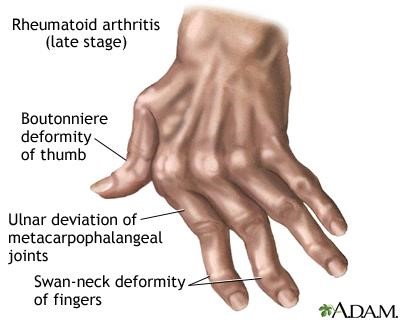 The synovium becomes thickened and inflamed, and fluid accumulates in the joint space; this causes a pannus to form.
The synovium becomes thickened and inflamed, and fluid accumulates in the joint space; this causes a pannus to form.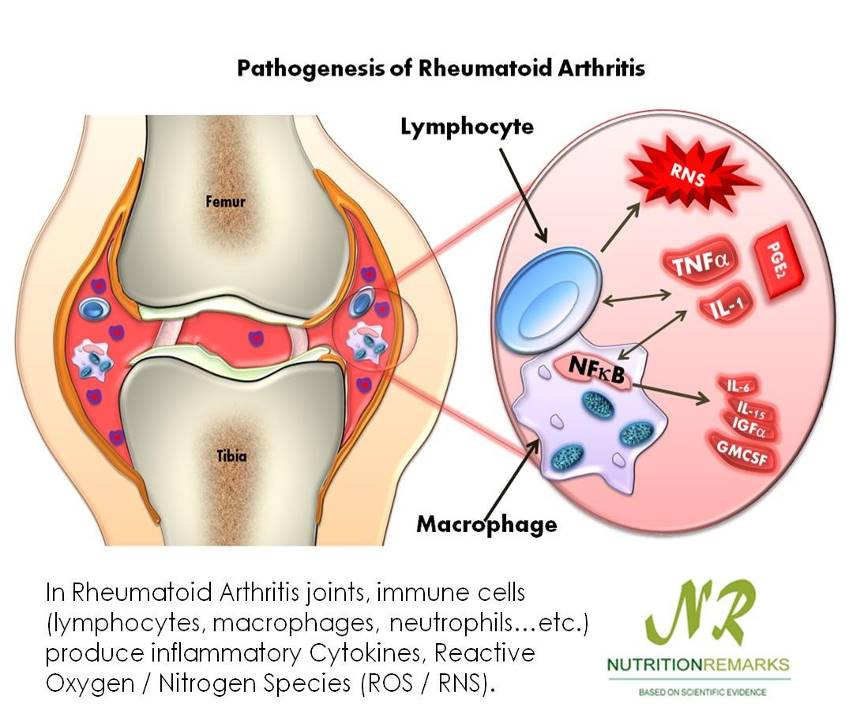 Painful when moved.
Painful when moved.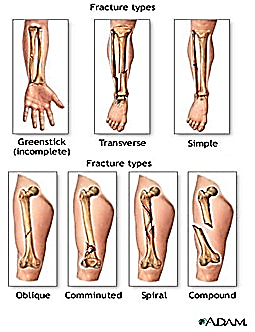 with elbows straight, there is a high incidence of neurovascular complications due to the anatomic relationship of the brachial artery and nerves to the fracture site.
with elbows straight, there is a high incidence of neurovascular complications due to the anatomic relationship of the brachial artery and nerves to the fracture site.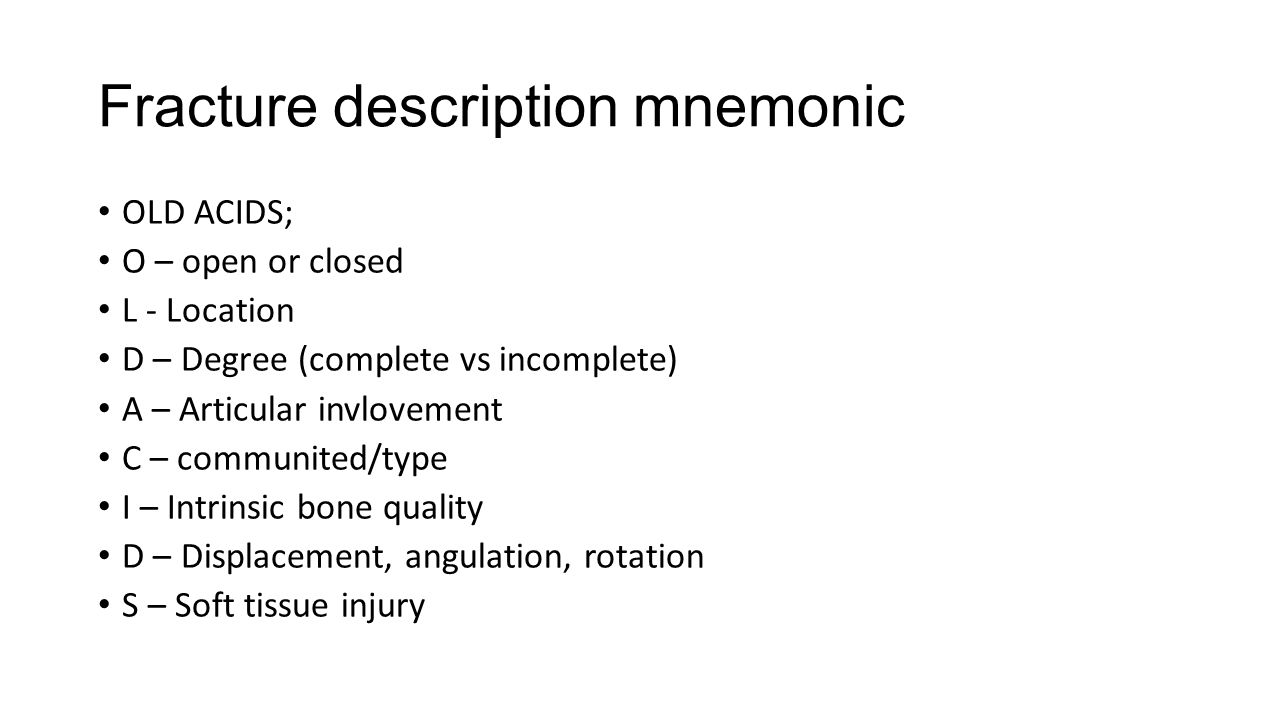
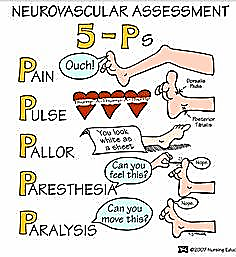 Other characteristic findings include deformity, swelling, bruising, muscle spasms, tenderness, pain, impaired sensation, loss of function, abnormality, crepitus, shock or refusal to walk (in small children).
Other characteristic findings include deformity, swelling, bruising, muscle spasms, tenderness, pain, impaired sensation, loss of function, abnormality, crepitus, shock or refusal to walk (in small children).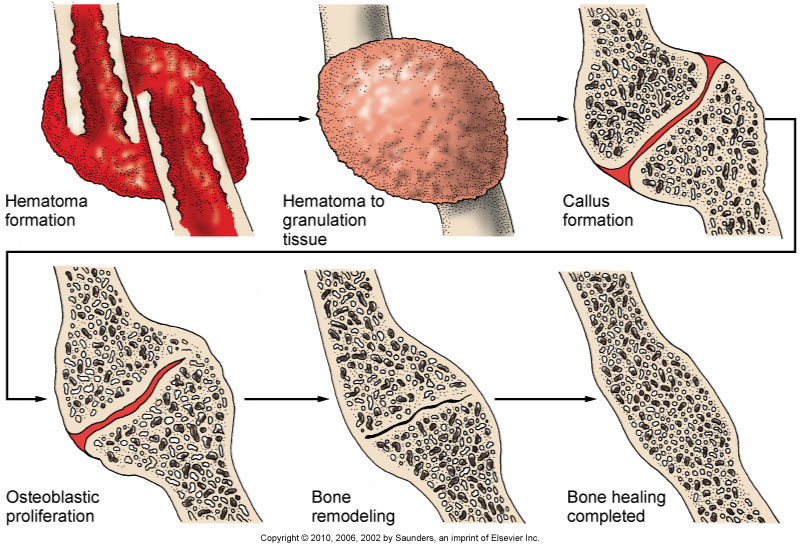

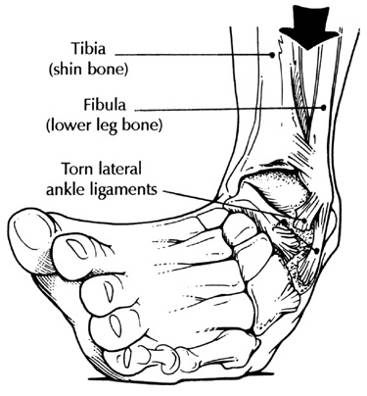 A Sprain is a torn ligament. The area around the affected joint becomes Swollen, and painful. Sprains occur most in the ankles, wrist, fingers and knees.
A Sprain is a torn ligament. The area around the affected joint becomes Swollen, and painful. Sprains occur most in the ankles, wrist, fingers and knees.