
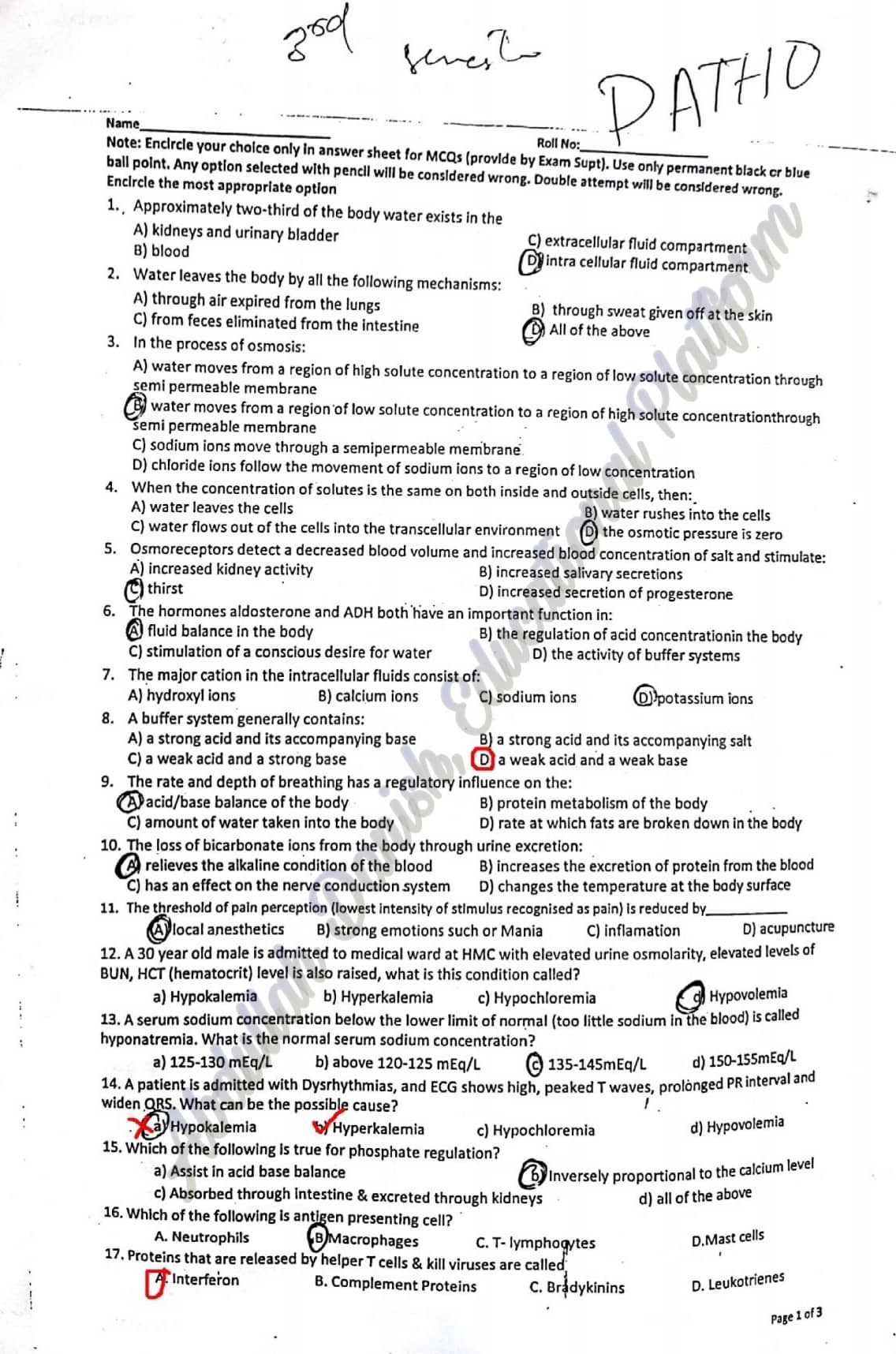
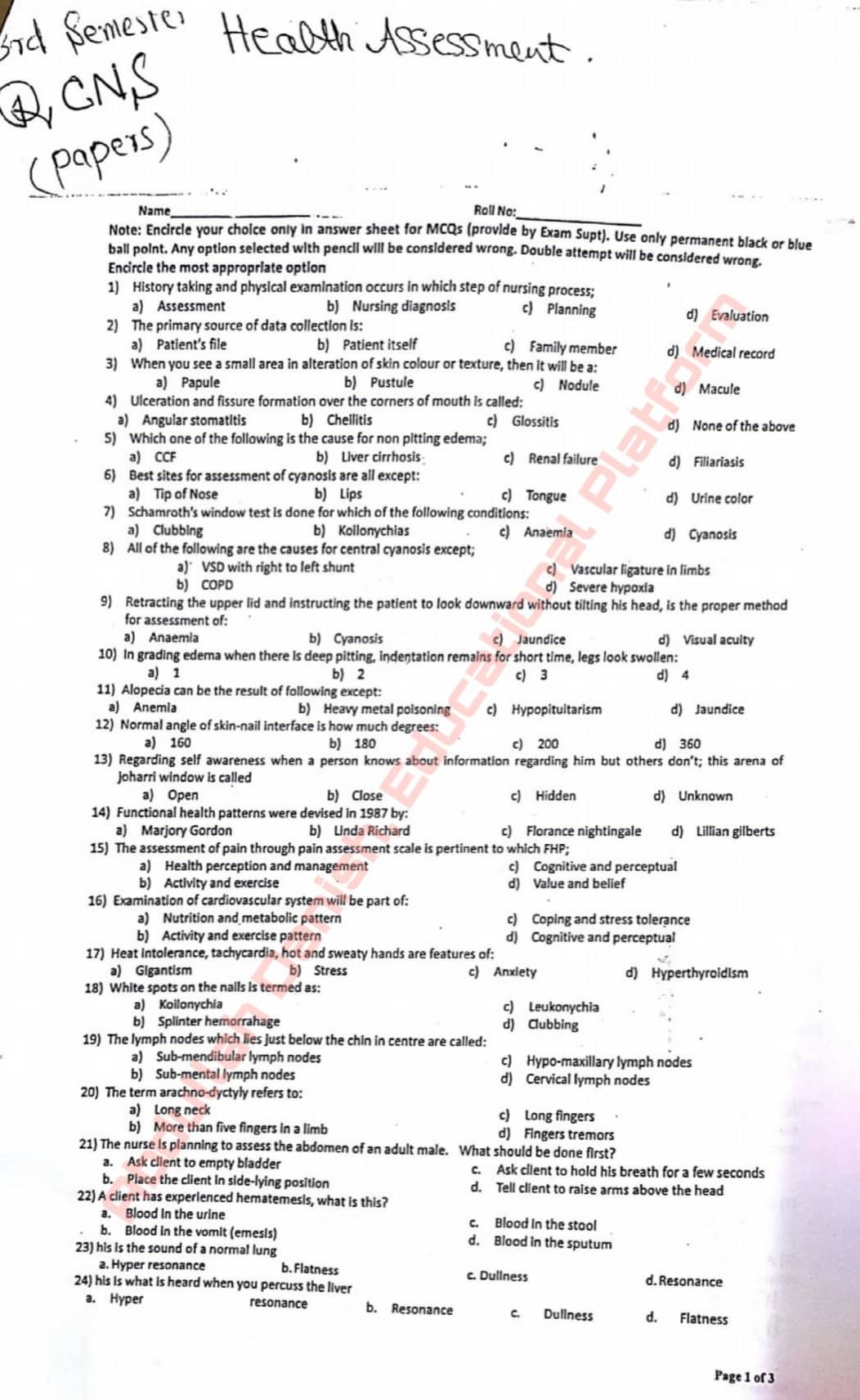
1) When doing an assessment on a client’s eyes the very first thing that a nurse should look at is?
A. Eye internal structures
B. Eye external structures
C. The pupils reactivity to light
D. Color of the irises of the eye
2) While the nurse is inspecting the throat of a client with a tongue blade, the client begins to gag. What does this response indicate to the nurse?
A. The client is nauseated.
B. The client has nerve damage to his tongue.
C. The client has a functioning response.
D. The client has a malfunctioning response
3) During the health history, a client begins to talk about her dog and the trouble she is having housebreaking the new pet. To help the client return to the health interview, the nurse could use the communication skill:
A. Listening
B. Reflecting
C. Questioning
D. Focusing
4) After inspecting a client’s abdomen, which assessment technique should the nurse use next?
A. Light Palpation
B. Percussion
C. Auscultation
D. Deep Palpation
5) Nurse Tara asks her client Farhan to clench his jaw as she continues to palpate his head. When she asks him to do this what is Nurse Tara most likely trying to palpate?
A. Faran’s submandibular joint
B. Farhan’s submental joint
C. Farhan’s temporomandibular joint
D. Faran’s temporal artery
6) The nurse is planning to palpate a client’s bladder. Which area of the abdomen should this palpation be done?
A. Hypogastric region
B. Right hypochondriac region
C. Right Lower Quadrant
D. Left lumbar region
7) A 70-year-old male client comes into the clinic with weight loss and difficulty swallowing. Which of the following should the nurse document for this client?
A. Odynophagia
B. Bulimia
C. Dysphagia
D. Aphasia
8) A 15-year-old high school student came to the clinic with a 1-day history of nausea and anorexia. He describes the pain as generalized yesterday, but today it has localized to the right lower quadrant. You palpate the left lower quadrant and the patient experiences pain in the right lower quadrant. What is the name of this sign?
A. Murphy’s sign
B. Psoas sign
C. Grey Turner’s sign
D. Rovsing’s sign
9) During eye assessment when you asked the patient to follow your finger or pencil as you move it in toward the bridge of the nose. Which of the following test you are performing?
A. Visual acuity
B. Visual Fields by Confrontation
C. Test for convergence
D. Visual fields
10) A nurse doing her assessment proceeds to palpate a client’s frontal and maxillary sinuses. What should she make sure she checks for?
A. Tactile signs of carcinoma
B. Swelling
C. Lesions
D. Tenderness
11) A nurse would use either a Snelling chart or the finger wiggle test to assess a client’s what?
A. Hearing
B. Vision
C. Consensual light reflex
D. Bone conduction
12) During assessment of pharynx you as the client to say “Ah” and uvula and soft palate rise centrally. It determines the function of which cranial nerve:
A. Spinal accessory
B. Vagus
C. Trochlear
D. Trigeminal
13) During the assessment of a client, the nurse gently touches the tip of a sterile cotton swab in the client’s eye. Which of the following would be considered an expected response for the client to make?
A. Begin sneezing.
B. Blink.
C. Scream in pain.
D. Swat the nurse’s hand away.
14) If assessing a client for kidney tenderness, where would you begin?
A. External Oblique Angle
B. Left Upper Quadrant
C. Right Upper Quadrant
D. Costovertebral Angle
15) The three things a nurse needs to check for when doing an examination on the eyes regarding the external structures is?
A. Eyelash texture, shape of eyes, redness
B. Shape of eyes, pupils reactivity, iris’s color
C. Drainage, possible tumors, irritation
D. Eyelash distribution, coloring, drainage
16) A 40-year-old female came for evaluation of abdominal pain. She stated that it is worse after eating, especially if she has a meal that is spicy or high in fat. She has taken antacids, but they have not helped the pain. After examining her abdomen, you strongly suspect cholecystitis. Which sign on examination increases your suspicion for this diagnosis?
A. Murphy’s sign
B. Psoas sign
C. Grey Turner’s sign
D. Rovsing’s sign
17) During the percussion of a client’s abdomen, the nurse hears a loud high-pitched drum like tone. The nurse would document this sound as being:
A. Resonance
B. Tympany
C. Hyper-resonance
D. Flatness
18) What could the nurse assess based solely on the way the client walks into the room?
A. Signs of illness, well nourished
B. Dress and signs of illness
C. Gender and age
D. Gait and posture
19) Which of the following is a clinical manifestation of Bell’s palsy?
A. Asymmetry of the mouth
B. Asymmetry of the entire side of the face
C. Asymmetry of the lower face
D. Involuntary movements of the face
20) The nurse notices that a client walks with a limp and has long legs. Which of the following aspects of the general survey is this nurse assessing?
A. Physical appearance
B. Behavior
C. Mental status
D. Mobility
21) Test for shifting dullness is performed to assess:
A. Liver abscess
B. Ascites
C. Cholecystitis
D. Peritonitis
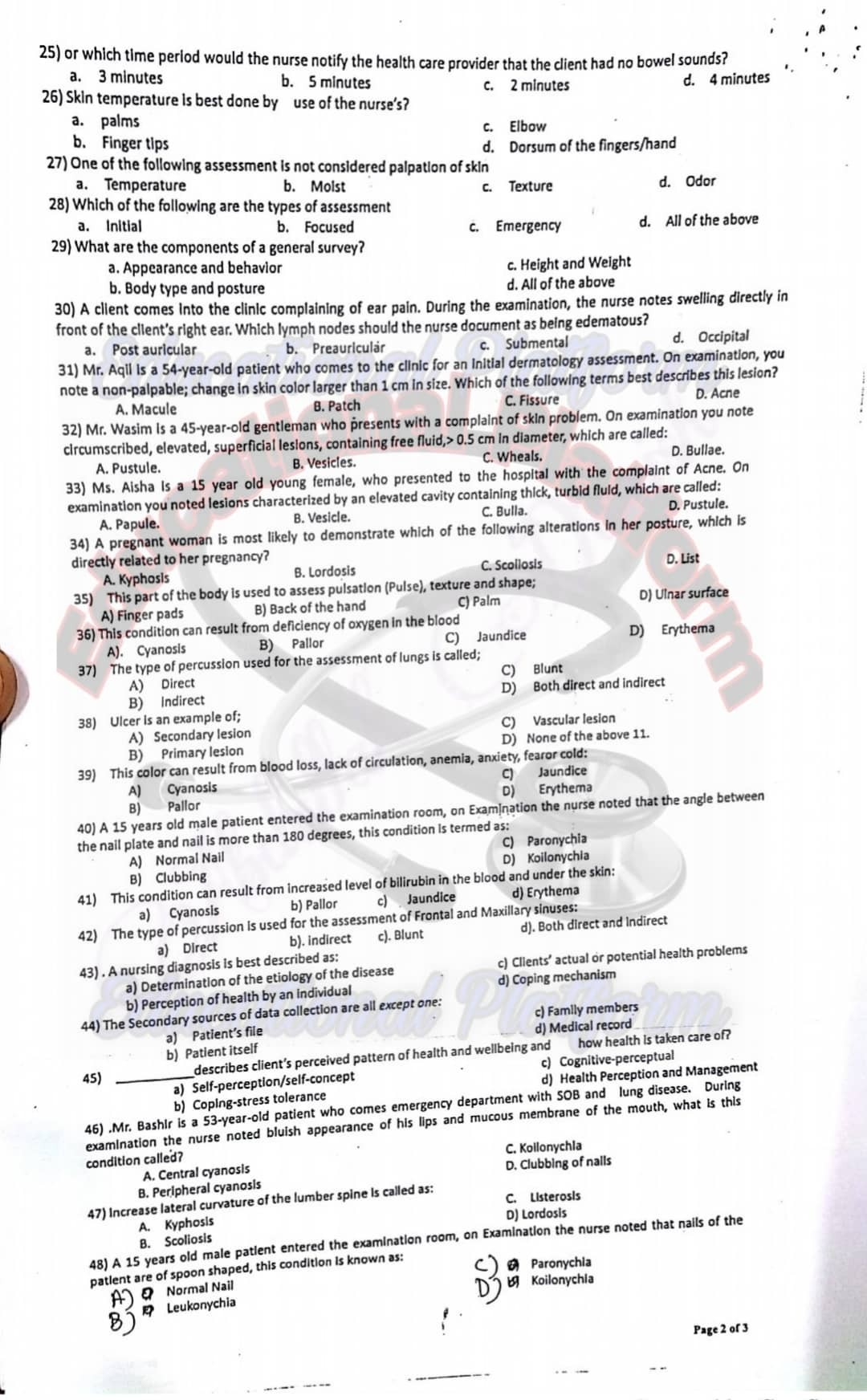
22) When a nurse performing the eye examinations, which piece of equipment does she/he use to inspect the eye structures?
A. Ultrasonic stethoscope
B. Sphygmomanometer
C. Ophthalmoscope
D. Otoscope
23) The normal liver span of an adult is:
A. 7-12 cm
B. 5-12 cm
C. 6-12 cm
D. 4-12 cm
24) A client comes into the clinic for a routine breast and axilla exam. Which assessment technique does the nurse use first during this examination?
A. Palpation
B. Auscultation
C. Inspection
D. Percussion
25) The clinic is sponsoring a client education session for breast cancer awareness month. Which of the following considerations should be included to support cultural differences about breast health?
A. Refer all clients to the American Cancer Society if they have questions.
B. Inform all about the low-cost breast cancer screening program…
C. A:
D. Encourage all females to increase their intake of vitamins A and E
26) Grade +2 pitting edema is:
A. 4 mm deep
B. 6 mm deep
C. 2 mm deep
D. 8 mm deep
27) The nurse is going to assess a client’s blood pressure. To do this, the nurse will need to have:
A. A stethoscope and sphygmomanometer
B. A tongue blade and tuning fork
C. A flashlight and gloves
D. A stethoscope and thermometer
28) The clinic is sponsoring a client education session for breast cancer awareness month. Which of the following considerations should be included to support cultural differences about breast health?
A. Refer all clients to the American Cancer Society if they have questions.
B. Encourage all females to increase their intake of vitamins A and E.
C. Inform all about the low-cost breast cancer screening program.
D. Encourage all females to complete monthly breast exams
29) After auscultating the bowel sounds of a client, the nurse realizes the sounds were long. Which of the following would be appropriate for the nurse to use to document this finding?
A. Intensity
B. Pitch
C. Quality
D. Duration
30) During the physical assessment of Mr. Ahsan’s skin, the nurse observed that Mr. Ahsan’s skin color is pale, the nurse expect that Mr. Ahsan may has:
A. Jaundice
B. Anemia
C. Heart failure
D. Pulmonary edema
31) The nurse assesses a client’s vision to be 20/150. The client asks for an explanation of the numbers. Which of the following would be a correct explanation for the nurse to say to the client?
A. You might need surgery to correct the nystagmus
B. You see at 20 feet what a person with normal vision sees at 150 feet.
C. You see at 150 feet what a person with normal vision sees at 20 feet.
D. You have impaired vision
32) A nurse conducting an assessment on a client’s head would do what first?
A. Inspect and palpate hair
B. Look at patient’s prior medical history
C. Inspect and palpate scalp
D. Inspect and palpate sinuses to control spread of germs
33) The nurse is planning to assess the abdomen of an adult male.
A. Place the client in side-lying position
B. Ask client to empty bladder
C. Tell client to raise arms above the head
D. Ask client to hold his breath for a few seconds
34) Normal angle at nail base is:
A. 10 degrees
B. 160 degrees
C. 180 degrees
D. 30 degrees
35) When performing an ear assessment, the nurse notes tenderness of the pinna and tragus to movement and the presence of drainage in the external canal. The nurse suspects which of the following?
A. Otitis Media
B. Otitis Externa
C. An inner ear infection
D. A negative rmberg’s sign
36) The nurse asks the client to move his eyes in the shape of an H and then in a large X. The portion of the physical assessment the nurse is completing with this client is:
A. Assessing the optic nerve
B. Assessing extra ocular muscle movements
C. Assessing the eyelids
D. Assessing the red reflex
37) As the nurse introduces the otoscope into a client’s ear, the client starts to jerk his head and complains of pain. Which of the following should the nurse do?
A. Remove the otoscope and reinsert taking care not to touch the sides of the ear canal.
B. Begin to remove the embedded cerumen.
C. Instill ear drops.
D. Document “unable to complete the examination.
38) Which cranial nerve is affected by Bell’s palsy?
A. Facial (CN VII)
B. Trigeminal (CN V)
C. Vagus (X)
D. Abducens (CN VI)
39) In medical which term is used for “impaired near vision”?
A. Amblyopia
B. Myopia
C. Presbyopia
D. Diplopia
40) During the physical examination of a male client’s scrotum, the nurse palpates a mass. What should the nurse do next with this information?
A. Perform transillumination to further assess the finding.
B. Nothing. This is a normal finding.
C. Document mass palpated, left testicle.
D. Ask the client how long he’s had a tumor in his testicle.
41) During the breast exam, the nurse asks the client to raise her arms over her head. Why did the nurse change the client’s position?
A. The client has small breasts.
B. The client has large breasts.
C. The nurse couldn’t palpate the axillae correctly.
D. Skin dimpling is accented in this position
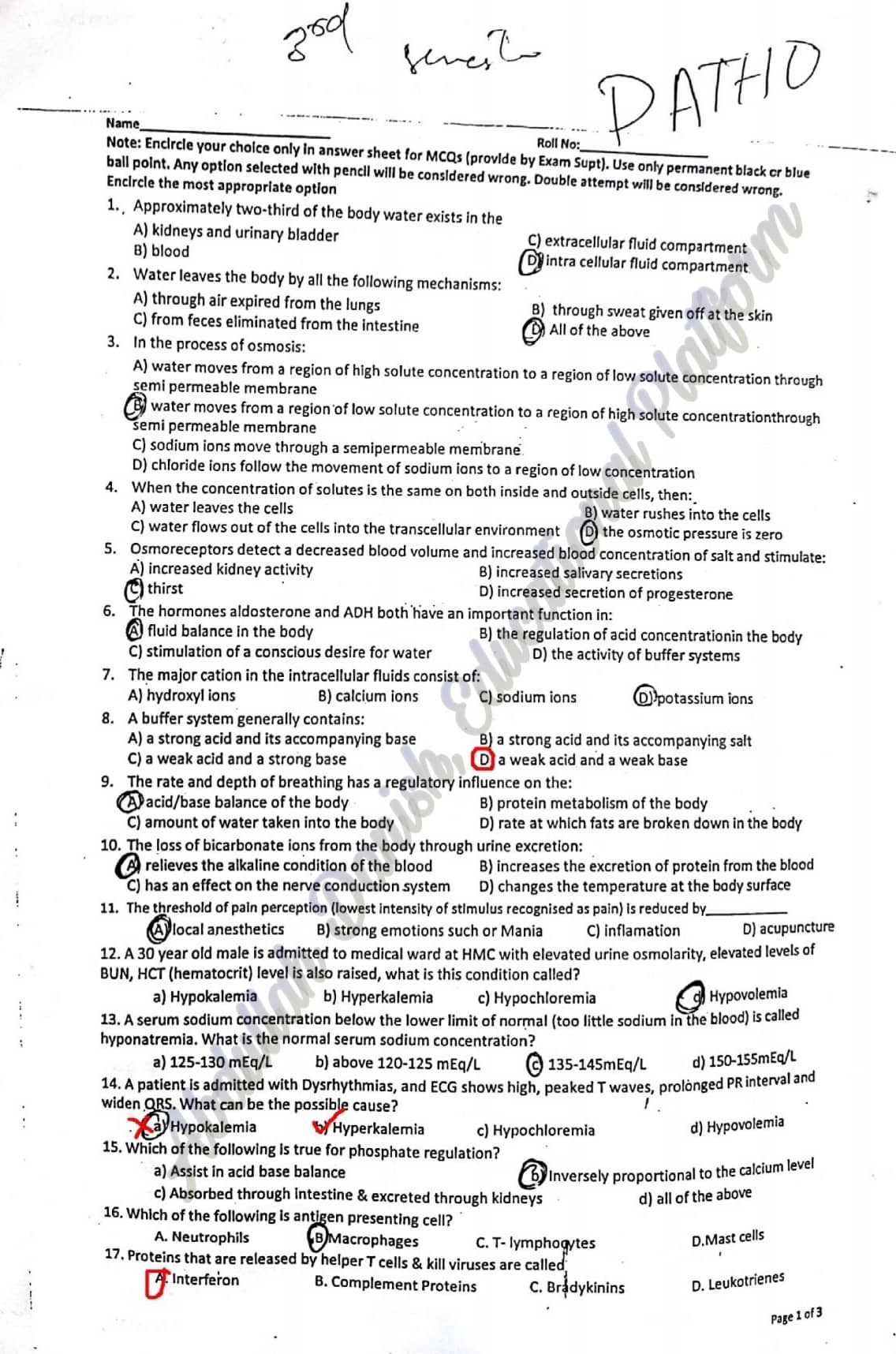
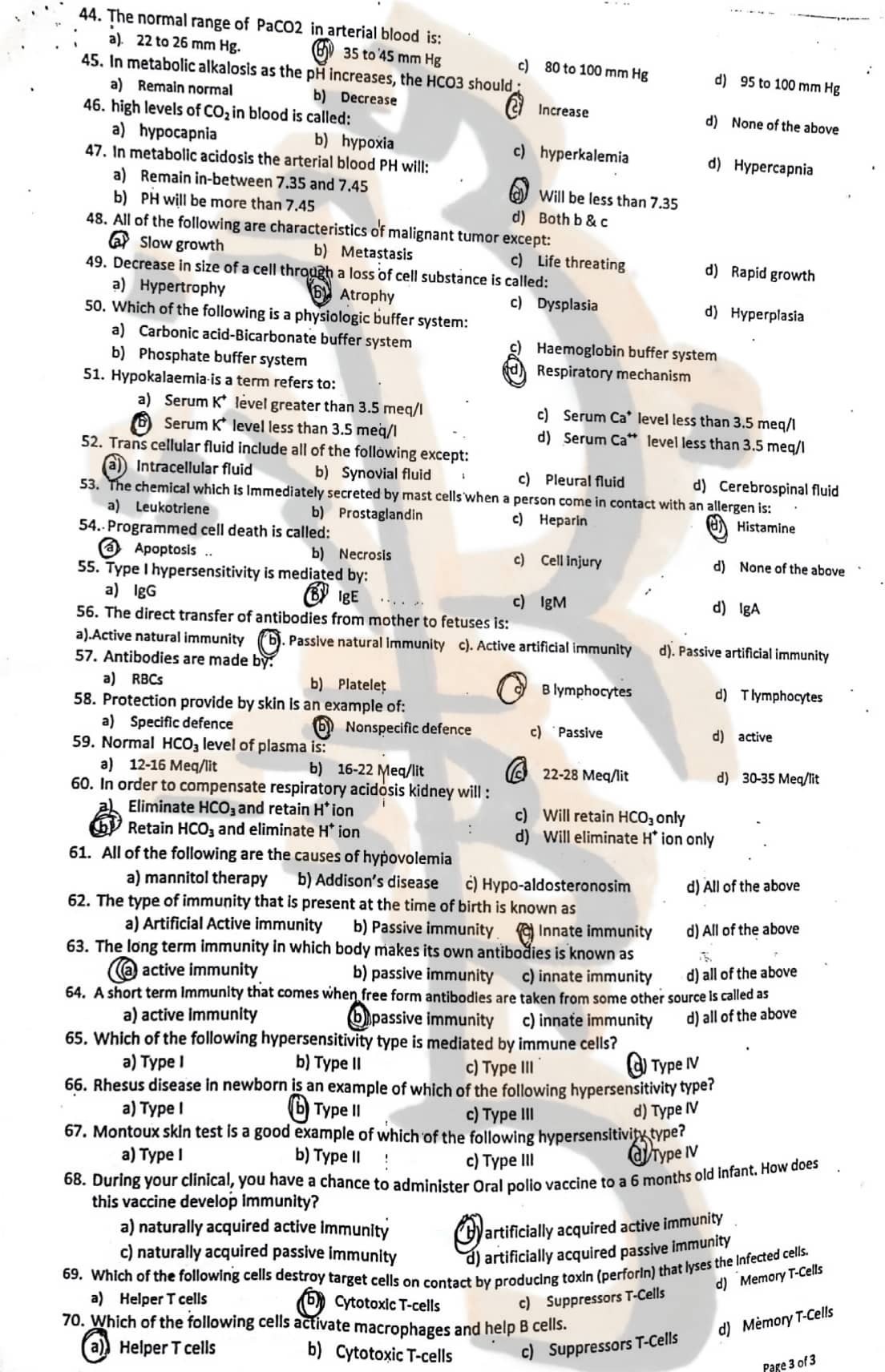
1) Total body water is:
1. 14L
2. 42L
3. 20 L
4. 28 L
2) All of the following are benign tumors, the most unlikely is:
1. Adenocarcinoma
2. Meningioma
3. Fibroma
4. Leiomyoma
3) Neutrophils predominate in acute inflammatory infiltrate during:
1. First 06 -24 hours
2. First 08 hours
3. First 04- 06 hours
4. First 24-48 hours
4) Most effective Bactericidal system in neutrophils is:
1. Halideion
2. MPOsystem (Myeloperoxidase)
3. NADPHoxidasesystem
4. MP0-H202Halidesystem
5) What is the most important prognostic factor for human cancer is proved to be of greater clinical value:
1. Stage
2. Vascular invasion.
3. Lymphocytic infiltration
4. Grade.
6) Most reliable feature that differentiates malignant tumor from benign is:
1. Local invasion
2. Metastasis
3. Irregular surface
4. Capsule
7) Regarding type – I hypersensitity:
1. Initial response is characterized by vasoconstriction
2. Late phase reaction occurs after few minutes
3. Develop after few days
4. Characterized by release of mast cell mediators
8) Reaction due to injection of horse serum (serum sickness) is example of:
1. Type – IV hypersensitivity
2. Type – Il hypersensitivity
3. Type – Ill hypersensitivity
4 Type – I hypersensitivity
9) Antibody mediated hypersensitivity does not occur in:
1. Erythroblastosis fetalis
2. Autoimmune Hemolytic anemia
3. Arthus reaction
4. Transfusion reaction
10) A 50 years old male develops sudden severe abdominal pain radiating to back. His lab values shows raised Amylase level. Regarding this case fat necrosis may occur in which of the following organ:
1. Brain
2. Skeletal muscle
3. Pancrease
4. Heart
11) Regarding Necrosis, which of the following statement is true:
1. Pancreas shows coagulative necrosis
2. Heart shows coagulative necrosis
3. Brain shows coagulation Necrosis
4. Heart shows liquefactive necrosis
12) In full term pregnancy, which one of the following cell adaptation has maximum contribution to increase in the size of uterus?
1. Dystrophy
2. Hyperplasia
3. Anaplasia
4. Atrophy
13) AIDS can be transferred through following factors except:
1.Inhalation
2. Blood
3. Direct contact
4. Saliva
14) All of the following are malignant tumors, the most unlikely is
1. Adenocarcinoma
2. Fibrosarcoma
3. Teratoma
4. Leukemia
16) Which of the following complement proteins may act as Opsonins:
1. c3b
2. C3a
3 C5b 9 complex
4. C3a & C5a
17) All of the following are malignant tumors, the most unlikely is:
1. Leukemia
2. Adenocarcinoma
3. Fibrosarcoma
4. Osteoma
18) Which one of the following mediator causes, chemotaxis of the leukocytes?
1. C1
2. C5a
3. c2a
4. C4
19) Granuloma with caseous necrosis is seen in:
1. Lymphoma
2. Tuberculosis
3. Sarcoidosis
4. Foreign body granuloma
20) Which of the following lab diagnostic technique is most convenient and suitable for the initial diagnosis and management of the patient suffering from swelling infront of neck (goiter)?
1 Smear
2. FNAC
3. Immunohistochemistry
4. Biopsy
21) ———— is also called Cytotoxic Hypersensitivity because it utilizes antibodies that can destroy normal cells by complement lysis or by antibody-dependent cellular cytotoxicity
1. Type-ll hypersensitivity
2. Type-l hypersensivitiy
3. Type-IV hypersensivitiy
4. Type-ll hypersensivitiy
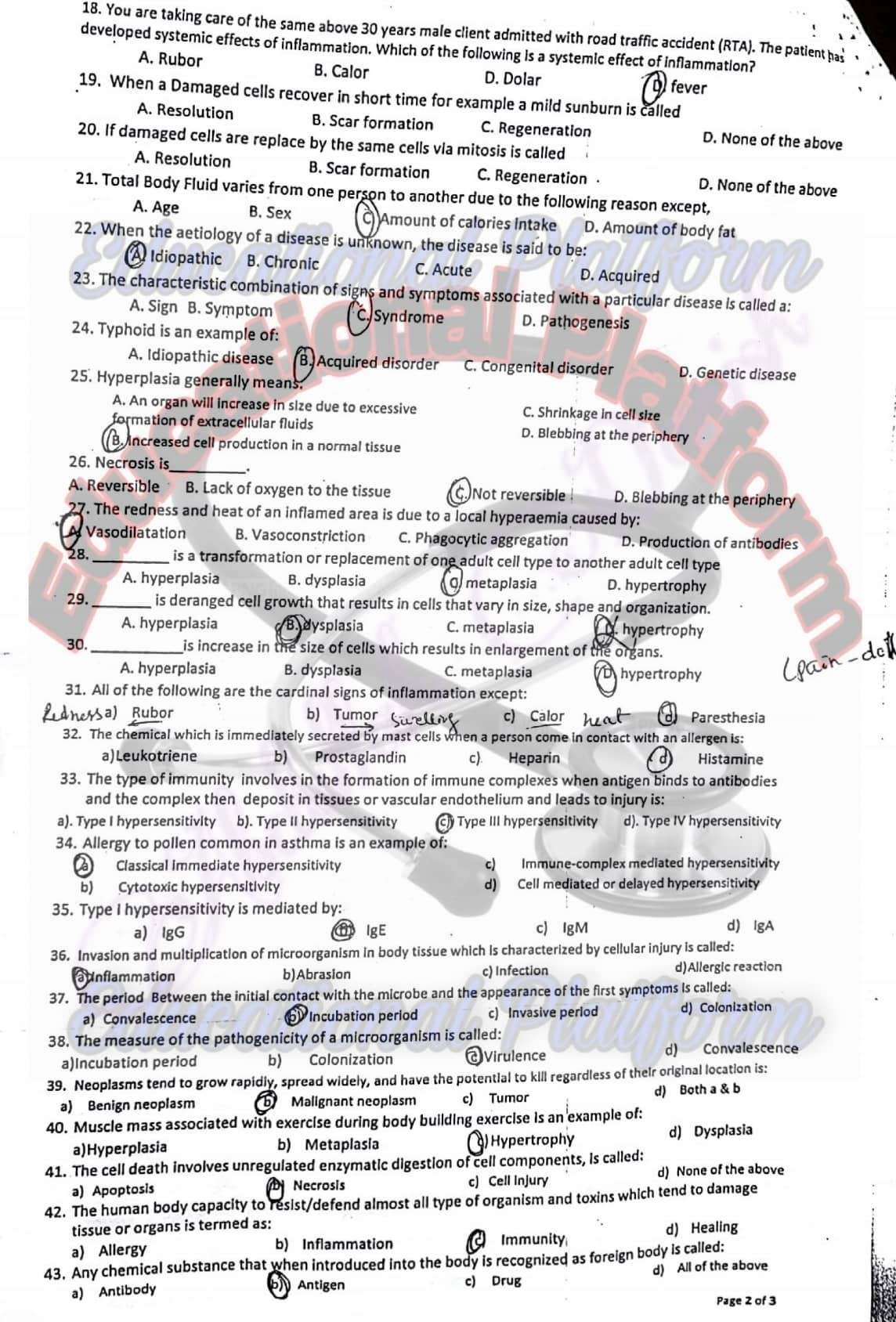
22) Most common chornic inflammatory cells are:
1. Neutrophils
2. Macrophages
3. Eosinophils
4. Plasma cells
23) Malignant tumor arising from mesenchymal tissue is most likely called as:
1. Adenomna
2. Sarcoma
3. Hepatoma
4. Fibroma
24) Metastasis of cancer most unlikely occur by:
1. Lymphatic spread
2. Direct seeding of body cavities
3. Aerosol droplet
4. Hematogenous spread
25) Regarding anaplasia which of the following statement is true:
1. Nuclear to cytoplasmic ratio 1:6
2. Increase mitosis
3. Well differentiated cells
4. Normal size of shape of cells
26) Laboratory test most commonly used for diagnosis of AIDS is:
1. ELISA
2. EASTERN BLOT
3. RIBA
4. WESTERN BLOT
27) Multiple sclerosis is example of:
1. Type – l hypersensitivity
2. Type- IV hypersensitivity
3. Type-Ill hypersensitivity
4. Type – I hypersensitivity
28) Generalized edema through the body is termed as:
1. Anasarca
2. Anaplasia
3. Sarcoma
4. Pitting edema
29) Major component of innate immunity are all of following, the most unlikely is:
1. Epithelial barrier
2. B-lymphocyte
3. Complement proteins
4. NK cells
30) A 40 years old male suffering from cervical lymphadenopathy. Biopsy report shows granuloma with caseous necrosis. The most likely diagnosis will be
1. Tuberculosis
2. Sarcoidosis
3. Lymphoma
4 Foreign body granuloma
31) Pathological hyperplasia of thyroid gland occurs in:
1. Thyroid connective tissue
2. Thyroid follicles
3. Whole thyroid tissue
4. Thyroid stroma
32) A 55 years old female with ovarian Carcinoma developed ascities. Cytological analysiss of ascitic fluid show malignant cells. Which of the following pathway best explaining the spreading of tumor to the peritonium:
1. Seeding of body cavity
2. Lymphatic spread
3. Hematogenous spread
4. Direct Extension
33) Weakness and wasting of the body due to severe chronic illness is referred to:
1. Neoplasm
2. Cachexia
3. Anorexia
4. Fatigue
34) Which of the following is earliest stage of vascular events of acute inflammation?
1. Vasodilation
2. Initial vasoconstriction
3. Redness
4. Leukocytic migration
35) Increased concentration of potassium in the blood is termed as:
1. Hypernatremia
2. Hyperkalemia
3. Hypokalemia
4. Hyponatremia
36) Loss of uniformity of cells & Ioss of arachitectural orientation is most likely called as:
1. Desmoplasia
2. Metaplasia
3. Dysplasia
4. Anaplasia
37) Arthus reaction is example of:
1. Type – lll hypersensitivity
2. Type – II hypersensitivity
3. Type- IV hypersensitivity
4. Type – I hypersensitivity
38) All are causes of atrophy, the most unlikely is:
1. Diminished blood supply
2. Denervation
3. Decrease workload
4. Increase workload
39) Excessive intake of acid containing foods and beverages may lead to development of:
1. Metabolic acidosis
2. Respiratory alkalosis
3. Metbolic alkalosis
4. Respiratory acidosis
40) In full term pregnancy, which one of the following cell adaptations has maximum contribution to increase in the size of uterus?
1. Dystrophy
2. Hyperplasia
3. Anaplasia
4 Atrophy
41) Goodpasture syndrome is example of:
1. Type -Ill hypersensitivityy
2. Type – I hypersensitivity
3. Type-ll hypersensitivity
4. Type – IV hypersensitivity
Q1) Explain Strategies for managing patient with urinary stress incontinence
Ans :- The nurse instructs the patient to:
1)Avoid bladder irritants, such as caffeine, alcohol, and aspartame (NutraSweet).
2)Avoid taking diuretic agents after 4 pm.
3)increased awareness of the amount and timing of all fluid intake.
4)Perform all pelvic floor muscle exercises as prescribed, every day.
5)Stop smoking (smokers usually cough frequently, which increases incontinence).
6)Take steps to avoid constipation: Drink adequate fluids, eat a well-balanced diet high in fiber, exercise regularly, and take stool softeners if recommended.
7)Void regularly, 5–8 times a day (about every 2–3 hours):
Q2) a) difference between AIDS and HIV
HIV:
HIV (Human Immunodeficiency Virus)
HIV is the acronym for human deficiency virus
Virus that invades the immunity system
Patient may suffer minor difficulties; symptoms will be similar to flu
AIDS:
AIDS (acquired immunodeficiency syndrome)
AIDS is the acronym for acquired immune deficiency syndrome
Large stage of spectrum of conditions, initially caused by the infection of (HIV)
Patient will experience severe sign and symptoms, disrupting the quality of life
Prevention of HIV
Individuals can reduce the risk of HIV infection by limiting exposure to risk factors.
1)Male and female condom use before sex
2)Testing and counselling for HIV and STIs
3)Testing and counselling, linkages to tuberculosis (TB) care
4)Avoid sharing contaminated needles, syringes and other injecting equipment and drug solutions when injecting drugs
5)Elimination of mother-to-child transmission of HIV
Q3) enlist types of hypersensitivity and explain management of any one of them And :- Definition
Hypersensitivity is an excessive or aberrant immune response to any type of stimulus
Types of hypersensitivity
1)Anaphylactic (Type I) Hypersensitivity
2)Cytotoxic (Type II) Hypersensitivity
3)Immune Complex (Type III) Hypersensitivity
4)Delayed-Type (Type IV) Hypersensitivity
Anaphylactic (Type I) Hypersensitivity Management
1)Antihistamines actto block the effects of histamine, which reduces vascular permeability and bronchoconstriction.
2)Corticosteroids which can be used to reduce the inflammatory response, as well as epinephrine, which is sometimes given during severe reactions via intramuscular injections through an EpiPen or intravenousinjection.
3)Epinephrinecan help constrict blood vessels and prevent anaphylactic shock.
Q4) enlist complication of chemotherapy
Ans :- Complication of chemotherapy
Q5) explain immediate post operative care of patient after appendectomy Ans :-
Post Operative care
1)Monitor vital sign.
2)Assess level of consciousness.
3)Assess bleeding at wound site.
4)Give clear fluid for first POD.
5)Monitor for infection and any complication at the wound incision.
6)Administer IV prophylaxis antibiotics as ordered.
7)Maintain aseptic technique during dressing.
8)Encourage patient to do ROM exercise.
Q6) English types of abortion and explain management of any one Ans :- Definition
Interruption of pregnancy or expulsion of the product of conception before the fetus is viable is called abortion. The fetus is generally considered to be viable any time after the fifth to sixth month of gestation.
Types of abortion
1)Threatened abortion:-
The term threatened abortion is used when a pregnancy is complicated by vaginal bleeding before the 20th week. Pain may not be a prominent feature of threatened abortion, although a lower abdominal dull ache sometimes accompanies the bleeding. Vaginal examination at this stage usually reveals a closed cervix. 25% to 50% of threatened abortion eventually result in loss of the pregnancy.
Management
The patient is kept at rest in bed until 2 days after blood loss has ceased. Intercourse is forbidden. As soon as the initial bleeding has stopped an ultrasound scan is performed. This will reveal whether or not the pregnancy is intact. The prognosis is good when all abnormal signs and symptoms disappear and when the resumption of the progress of pregnancy is apparent.
2)Inevitable abortion:-
In case of inevitable abortion, a clinical pregnancy is complicated by both vaginal bleeding and cramp-like lower abdominal pain . The cervix is frequently partially dilated, attesting to the inevitability of the process.
Management
The uterus usually expels its contents unaided , and examination must be made with strict aseptic technique. If the abortion is not quickly completed, or if hemorrhage becomes severe, the contents of the uterus are removed with a suction curettege.
3)Incomplete Abortion:-
In addition to vaginal bleeding, cramp-like pain, and cervical dilatation , an incomplete abortion involves the passage of products of conception , often described by the women as looking like pieces of skin or liver.
Management
Patients require admission to the hospital. Treatment is aimed at preventing infection, controlling bleeding and obtaining an empty and involuting uterus. The chief risks associated with retained products are hemorrhage and sepsis.
4)Missed Abortion: –
The term missed abortion is used when the fetus has died but is retained in the uterus, usually for some weeks. After 16 weeks’ gestation, dilatation and curettage may become a problem. Fibrinogen levels should be checked weekly until the fetus and placenta are expelled.
Management
Once the diagnosis has been made the uterus should be emptied. Early in gestation evacuation of the uterus is usually accomplished by suction curettage. The prognosis for the mother is good. Serious complications are uncommon.
5) Recurrent Abortion: –
Recurrent abortion refers to any case in which there have been three consecutive spontaneous abortions. Possible causes are known to be genetic error, anatomic abnormalities of the genital tract, hormonal abnormalities, infection, immunologic factors, or systemic disease.
Management
Paternal and maternal chromosomes should be evaluated. The mother should be ruled out the presence of systemic disorders such as DM, SLE, and thyroid disease. It should rule out the presence of Mycoplasma, Listeria, Toxoplasma etc. infectious disease. Pelvic examination
Q7) English types of abortion and explain management of them
Types of abortion
1)Threatened abortion
2)Inevitable abortion
3)Incomplete Abortion
4)Missed Abortion
5)Recurrent Abortion
Q1) a) define Folic acid deficiency anemia.
Folate-deficiency anemia is a decrease in red blood cells (anemia) due to a lack of folate. Folate is a type of vitamin B. It is also called folic acid. Anemia is a condition in which the body does not have enough healthy red blood cells. Red blood cells provide oxygen to body tissues.
b) write down the dietary sources of Folic acid
c) write down the importance of Folic acid in human body
1)Folic acid helps your body produce and maintain new cells.
2)It helps prevent changes to DNA that may lead to cancer.
3)As a medication, folic acid is used to treat folic acid deficiency and certain types of anemia (lack of red blood cells) caused by folic acid deficiency.
Q2) a) define appendicitis
It is an acute inflammation of vermiform appendix (a small finger like appendage attached to caecum just below the ileocecal valve)
Q3) define ovarian cyst
Ovarian cysts are fluid-filled sacs or pockets in an ovary or on its surface. Women have two ovaries, each about the size and shape of an almond on each side of the uterus.
Management
▪ Functional/physiologic cysts usually resolve spontaneously
MEDICATIONS
SURGERY
Laparoscopy/laparotomy
Q4) define polycythemia
Polycythemia refers to an increase in the number of red blood cells in the body. The extra cells cause the blood to be thicker, and this, in turn, increases the risk of other health issues, such as blood clots.
Primary Polycythemia occurs when excess red blood cells are produced as a result of an abnormality of the bone marrow. Often, excess white blood cells and platelets are also produced.
Secondary polycythemia is usually due to increased erythropoietin (EPO) production either in response to chronic hypoxia (low blood oxygen level) or from an erythropoietin secreting tumor.
Relative erythrocytosis is an increase in RBC numbers without an increase in total RBC mass. Usually, this is caused by loss of plasma volume with resultant hemo-concentration, as seen in severe dehydration related to vomiting and diarrhea.
Stress polycythemia is a term applied to a chronic (long standing) state of low plasma volume, which is seen commonly in active, hardworking, anxious, middle-aged men. In these people, the red blood cell volume is normal, but the plasma volume is low.
Q5) a) define infertility
Inability to achieve pregnancy with limited intercourse for at least 1 year
1)The most common overall cause of female infertility is the failure to ovulate.
2)Problems with the menstrual cycle, the process that prepares the female body for pregnancy, can lead to infertility.
3)Structural problems usually involve the presence of abnormal tissue in the fallopian tubes or uterus.
4)Infections can also cause infertility in men and women.
5)Implantation failure refers to the failure of a fertilized egg to implant in the uterine wall to begin pregnancy.
6)Polycystic Ovary Syndrome (PCOS) is one of the most common causes of female infertility.
7)Primary Ovary Insufficiency (POI) is a condition in which a woman’s ovaries stop producing hormones and eggs at a young age.
8)Autoimmune disorders cause the body’s immune system to attack normal body tissues it would normally ignore. Autoimmune disorders, such as lupus, Hashimoto’s and other types of thyroiditis, or rheumatoid arthritis, may affect fertility.
Causes of infertility in Males
1)Sperm Disorders
The most common problems are with making and growing sperm. Sperm may:
2)Varicoceles
Varicoceles are swollen veins in the scrotum. They harm sperm growth by blocking proper blood drainage.
3)Retrograde Ejaculation
Retrograde ejaculation is when semen goes backwards in the body. They go into your bladder instead of out the penis. This happens when nerves and muscles in your bladder don’t close during orgasm (climax). Semen may have normal sperm, but the semen cannot reach the vagina.
4)Immunologic Infertility
Sometimes a man’s body makes antibodies that attack his own sperm.
5)Obstruction
Sometimes sperm can be blocked. Repeated infections, surgery (such as vasectomy), swelling or developmental defects can cause blockage. Any part of the male reproductive tract can be blocked. With a blockage, sperm from the testicles can’t leave the body during ejaculation.
6)Hormones
Hormones made by the pituitary gland tell the testicles to make sperm. Very low hormone levels cause poor sperm growth.
7)Chromosomes
Sperm carries half of the DNA to the egg. Changes in the number and structure of chromosomes can affect fertility. For example, the male Y chromosome may be missing parts.
8)Medication
Certain medications can change sperm production, function and delivery. These medications are most often given to treat health problems like:
Q6) a) define peritonitis
Inflammation of the peritoneum (The peritoneum is the tissue layer of cells lining the inner wall of the abdomen and pelvis). Peritonitis can result from infection (such as bacteria or parasites), injury and bleeding, or diseases (such as systemic lupus erythematosus).
Q7) write the short note on the following
1)CT scan
A computerized tomography (CT) scan combines a series of X-ray images taken from different angles around your body and uses computer processing to create cross-sectional images (slices) of the bones, blood vessels and soft tissues inside your body. CT scan images provide more-detailed information than plain X-rays do.
2) upper and lower endoscopies
Endoscopy is a procedure in which the gastrointestinal (GI) tract is viewed through a fiber-optic camera known as an endoscope, inserted either through the mouth (upper) to scan the esophagus, stomach and small intestines, or through the anus (lower) to examine the large intestine, colon and rectum.
3) parenthesis
Parenthesisrefer to punctuation marks “(” and “)” used to separate relevant information or a comment from the rest of the text, or to enclose mathematical symbols, or the text inside of these marks. The punctuation marks in the math equation 2x (4+6) are an example of parenthesis.
4) cystoscopy
Cystoscopy (sis-TOS-kuh-pee) is a procedure that allows your doctor to examine the lining of your bladder and the tube that carries urine out of your body (urethra). A hollow tube (cystoscope) equipped with a lens is inserted into your urethra and slowly advances into your bladder.
5) metabolic acidosis
Metabolic acidosis is a serious electrolyte disorder characterized by an imbalance in the body’s acid-base balance. Metabolic acidosis has three main root causes: increased acid production, loss of bicarbonate, and a reduced ability of the kidneys to excrete excess acids.
The most common causes of hyperchloremic metabolic acidosis are gastrointestinal bicarbonate loss, renal tubular acidosis, drugs-induced hyperkalemia, early renal failure, and administration of acids.
Q1) a) describe cirrhosis of liver
Cirrhosis of the liver is a chronic, progressive disease characterized by widespread fibrosis(scarring) and nodule formation.
The development of cirrhosis is an insidious, prolonged course, usually after decades of chronic liver disease.
b) enlist its signs and symptoms
Some of the more common symptoms and signs of cirrhosis include:
Q2) a) define intestinal obstruction and its types
This obstruction can involve only the small intestine (small bowel obstruction), the large intestine (large bowel obstruction), or via systemic alterations, involving both the small and large intestine (generalized ileus). The “obstruction” can involve a mechanical obstruction or, in contrast, may be related to ineffective motility without any physical obstruction, so-called functional obstruction, “pseudo-obstruction,” or paralytic ileus
There are two main types
b) describe its management and nursing care
1)Collaborative Care
a. Relieving pressure and obstruction
b. Supportive care
2)Gastrointestinal Decompression
a. Treatment with nasogastric or long intestinal tube provides bowel rest and removal of air and fluid
b. Successfully relieves many partial small bowel obstructions
3)Surgery
a. Treatment for complete mechanical obstructions, strangulated or incarcerated obstructions of small bowel, persistent incomplete mechanical obstructions
b. Preoperative care
1.Insertion of nasogastric tube to relieve vomiting, abdominal distention, and to prevent aspiration of intestinal contents
2.Restore fluid and electrolyte balance; correct acid and alkaline imbalances
3.Laparotomy: inspection of intestine and removal of infarcted or gangrenous tissue
4.Removal of cause of obstruction: adhesions, tumours, foreign bodies, gangrenous portion of intestines and anastomosis or creation of colostomy depending on individual case
4)Nursing Care
a. Prevention includes healthy diet, uid intake
b. Exercise, especially in clients with recurrent small bowel obstructions
Q3) a) define renal failure and its causes
A condition in which the kidneysstop working and are not able to remove waste and extra water from the blood or keep body chemicals in balance. Acute or severe renal failurehappens suddenly (for example, after an injury) and may be treated and cured.
The most common causes are:
Acute kidney failurehappens when your kidneyssuddenly lose the ability to eliminate excess salts, fluids, and waste materials from the blood. This elimination is the core of your kidneys’main function. Body fluids can rise to dangerous levels when kidneys lose their filtering ability.
Nursing Interventions:
10.Provide meticulous wound care.
11.Offer high-carbohydrate feedings because carbohydrates have a greater protein-sparing power and provide additional calories.
12.Institute seizure precautions. Provide padded side rails and have airway and suction equipment at the bedside.
13.Encourage and assist the patient to turn and move because drowsiness and lethargy may reduce activity.
14.Explain that the patient may experience residual defects in kidney function for a long time after acute illness.
15.Encourage the patient to report routine urinalysis and follow-up examinations.
16.Recommend resuming activity gradually because muscle weakness will be present from excessive catabolism.
Q4) a) what is abortion and describe its causes and types
Abortion is the termination of pregnancy before viability of the featus before 22 weeks or if the fetal weight is less than 500gm.
Or
Interruption of pregnancy or expulsion of the product of conception before the fetus is viable is called abortion. The fetus is generally considered to be viable any time after the fifth to sixth month of gestation.
Medical Management
After a spontaneous abortion, all tissue passed vaginally is saved for examination, if possible. The patient and all personnel who care for her are alerted to save any discharged material. In the rare case of heavy bleeding,the patient may require blood component transfusions and fluid replacement. An estimate of the bleeding volume can be determined by recording the number of perineal pads and the degree of saturation over 24 hours. When an incomplete abortion occurs, oxytocin may be prescribed to cause uterine contractions before D&E or uterine suctioning.
Nursing management
Because patients experience loss and anxiety, emotional support and understanding are important aspects of nursing care. Women may be grieving or relieved, depending on their feelings about the pregnancy. Providing opportunities for the patient to talk and express her emotions is helpful and also provides clues for the nurse in planning more specific care.
Q5) a) what is your understanding about infertility
Infertility is defined as a couple’s inability to achieve pregnancy after 1 year of unprotected intercourse
b) describe its pathophysiology and its management
Pathophysiology
Management
Q6) a) define anaemia
Anaemiais a condition in which you lack enough healthy red blood cells to carry adequate oxygen to your body’s tissues. Having anaemiacan make you feel tired and weak. There are many forms of anaemia, each with its own cause.
b) enlist its types
The seven types of anaemia
As the name implies, iron deficiency anemiais due to insufficient iron. Without enough iron, your body can’t produce enough of a substance in red blood cells that enables them to carry oxygen (hemoglobin). As a result, iron deficiency anemiamay leave you tired and short of breath.
Iron-Deficiency Anemia: Signs, Symptoms, and Treatment
To treat iron deficiency anemia, your doctor may recommend that you take iron supplements.
Iron supplements
Q7) differentiate between palliative care and hospice care
Q1) define first line defence /immune system
The first lineof defenceis your innate immune system. Level one of this system consists of physical barriers like your skin and the mucosal lining in your respiratory tract. The tears, sweat, saliva and mucous produced by the skin and mucosal lining are part of that physical barrier.
The bodys first line of defense against pathogens uses mostly physical and chemical barriers such as
Q2) define infertility and requirement for conception
In general, infertilityis definedas not being able to get pregnant (conceive) after one year (or longer) of unprotected sex. Because fertility in women is known to decline steadily with age, some providers evaluate and treat women aged 35 years or older after 6 months of unprotected sex.
The necessary requirements for conception to occur are the following:
Q3) describe types of metabolic acidosis
Metabolic acidosisis a serious electrolyte disorder characterized by an imbalance in the body’s acid-base balance. Metabolic acidosishas three main root causes: increased acid production, loss of bicarbonate, and a reduced ability of the kidneys to excrete excess acids.
Metabolic acidosis is classified into two types: Metabolic acidosis is classified into two types:
(a)metabolic acidosis with normal AG (with increased Cl ¯ ) and (a)metabolic acidosis with normal AG ( with increased Cl ¯ ) and (b) metabolic acidosis with high AG (with normal Cl ¯).
Q4) define abortion and types of abortion
Definition
Interruption of pregnancy or expulsion of the product of conception before the fetus is viable is called abortion. The fetus is generally considered to be viable any time after the fifth to sixth month of gestation.
Types of abortion
1)Threatened abortion:-
The term threatened abortion is used when a pregnancy is complicated by vaginal bleeding before the 20th week. Pain may not be a prominent feature of threatened abortion, although a lower abdominal dull ache sometimes accompanies the bleeding. Vaginal examination at this stage usually reveals a closed cervix. 25% to 50% of threatened abortion eventually result in loss of the pregnancy.
Management
The patient is kept at rest in bed until 2 days after blood loss has ceased. Intercourse is forbidden. As soon as the initial bleeding has stopped an ultrasound scan is performed. This will reveal whether or not the pregnancy is intact. The prognosis is good when all
abnormal signs and symptoms disappear and when the resumption of the progress of pregnancy is apparent.
2)Inevitable abortion:-
In case of inevitable abortion, a clinical pregnancy is complicated by both vaginal bleeding and cramp-like lower abdominal pain . The cervix is frequently partially dilated, attesting to the inevitability of the process.
Management
The uterus usually expels its contents unaided , and examination must be made with strict aseptic technique. If the abortion is not quickly completed, or if hemorrhage becomes severe, the contents of the uterus are removed with a suction curettege.
3)Incomplete Abortion:-
In addition to vaginal bleeding, cramp-like pain, and cervical dilatation , an incomplete abortion involves the passage of products of conception , often described by the women as looking like pieces of skin or liver.
Management
Patients require admission to the hospital. Treatment is aimed at preventing infection, controlling bleeding and obtaining an empty and involuting uterus. The chief risks associated with retained products are hemorrhage and sepsis .
4)Missed Abortion:-
The term missed abortion is used when the fetus has died but is retained in the uterus, usually for some weeks. After 16 weeks ’ gestation, dilatation and curettage may become a problem. Fibrinogen levels should be checked weekly until the fetus and placenta are expelled.
Management
Once the diagnosis has been made the uterus should be emptied. Early in gestation evacuation of the uterus is usually accomplished by suction curettage. The prognosis for the mother is good. Serious complications are uncommon .
5)Recurrent Abortion:-
Recurrent abortion refers to any case in which there have been three consecutive spontaneous abortions. Possible causes are known to be genetic error, anatomic
abnormalities of the genital tract, hormonal abnormalities, infection, immunologic factors, or systemic disease .
Management
Paternal and maternal chromosomes should be evaluated. The mother should be ruled out the presence of systemic disorders such as DM,SLE, and thyroid disease. It should rule out the presence of Mycoplasma, Listeria, Toxoplasma etc. infectious disease.Pelvic examination
Q5) define nursing intervention for patient with acute pancreatitis
Nursing Interventions
Q6) describe stomatitis and its nursing management
Stomatitis Definition : Stomatitis is an inflammation of the mucous lining of the mouth , which may involve the cheeks, gums ,tongue ,lips , and roof or floor of the mouth. The word“ stomatitis “ literally means inflammation of the mouth.
Nursing Management
Q7) define Hernia and types of hernia
Define Hernia
A condition in which part of an organ is displaced and protrudes through the wall of the cavity containing it (often involving the intestine at a weak point in the abdominal wall)
Types of hernia
1.) Inguinal hernia
i.) Indirect inguinal hernia
ii.) Direct inguinal hernia (in contrast)
2.) Hiatal Hernia
3.) Femoral hernias (protrude through the femoral ring)
4.) Umbilical hernia (congenital/acquire)
5.) Incisional/ventral hernias (occur at the site of previous surgical incision)
Types of Isolation
Strict isolation
Indication
Suspected Highly infection transmissible bacterial or virulent disease by direct or indirect contact and air born routes of transmission.
Requirements
Private room
Gown, mask, gloves, hand washing
Double bagged techniques for soiled articles.
Respiratory isolation
Private room
Gown, mask, gloves, hand washing
Patients with the same organism generally may share a room.
Labeled plastic bags are used for soiled articles.
Contact isolation
Indication
Infectious disease or multiple resistant microorganism that are spread by close or direct contact. Contact Precautions—used for infections, diseases, or germs that are spread by touching the patient or items in the room (examples: diarrheal illnesses, open wounds).
Requirements
Private room
Gown, mask, gloves, hand washing.
Enteric isolation/enteric precaution
Indication:
Infectious disease transmitted through
direct or indirect contact with infected feces.
Requirement:
A private room is required if the patient does not practice good hygiene measures.
Hand washing, gloves.
Gowns should only be worn when handling objects contaminated with feces.
Blood & body fluid precaution
Requirements
-Gloves, Mask, and protective eyes gear/cover.
-Gown
-Contaminated needles should not be recapped.
-Use puncture resistant containers for used needles and other sharp items.
Relate isolation to the chain of infection Cycle
Source: – patient, employee, Environment, Equipment, visitors.
Method of transmission: –
Air tune, vehicle, vector,
Contact: (direct, indirect).
Host: – Age, immunity, treatment, nutrition, disease, lifestyle, skin injury, socioeconomics condition.
Identify nursing responsibilities in each type of isolation
1.Aseptic techniques–
Always use aseptic technique any procedure in hospital
2. Isolation techniques-
Always use aseptic technique for the patient with communicable diseases (use of glove cap, Mask.
3. Fumigation-
Room and articles should be fumigation after death or discharge of patient with infectious disease or should be fumigated after specific interval.
4. Biological waste:
ward’s waste should be discarded in a proper way as per instruction.
5. Destruction of rodent and insects:
Rodent and insects also play a role in the spread of infection. They should be destroyed to prevent infection.
6. Hospital hygiene
The hospital should be well ventilated. The general cleanliness of the hospital maintained sweeping and mopping of the floor should be done, white washing of the walls windows, roofs, doors, should be done.
And other:
Droplet Isolation Precautions
MEDICAL & SURGICAL ASEPSIS
Purpose: a septic technique helps to prevent health care associated infection.
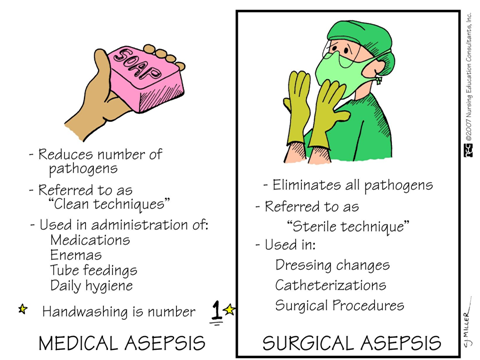
Types of Aseptic Technique
Medical or clean asepsis reduces the number of organisms and prevents their spread; surgical or sterile asepsis includes procedures to eliminate microorganisms from an area and is practiced by surgical technologists and nurses.
IDENTIFY THE 6 COMPONENTS OF CHAIN OF INFECTION
The spread of an infection within a community is described as a “chain,” several interconnected steps that describe how a pathogen moves about. Infection control and contact tracing are meant to break the chain, preventing a pathogen from spreading.
The transmission of infection depends on six elements which link together like chains.
The Spread of infection can be described as a chain with six components.
If any link is broken the chain is broken and infection cannot be transmitted.
1. The Infection Agent
(Pathogens) include not only bacteria but also viruses, fungi, and parasites. The virulence of these pathogens depends on their number, their potency, their ability to enter and survive in the body, and the susceptibility of the host. For example, the smallpox virus is particularly virulent, infecting almost all people exposed. In contrast, tuberculosis bacillus infects only a small number of people, usually people with weakened immune function, or those who are undernourished and living in crowded conditions.
Any disease-causing microorganisms (bacteria, virus, fungi, parasites etc).
2. The Reservoir
A reservoir is any person, animal, arthropod, plant, soil or substance (or combination of these) in which an infectious agent normally lives and multiplies. The infectious agent depends on the reservoir for survival, where it can reproduce itself in such manner that it can be transmitted to a susceptible host.
Where the germs normally live e.g. person, water, food, animal, plant, soil or substance feces, intravenous fluid, and equipment in which an infectious agent normally lives and multiplies.
3. The Portal of exist
A portal of exit is the means by which a pathogen exits from a reservoir. For a human reservoir, the portal of exit can include blood, respiratory secretions, and anything exiting from the gastrointestinal or urinary tracts.
Route by which the infectious micro-organism escapes or leaves the reservoir,
4. The Mode of transmission (Spread) route
People release respiratory fluids during exhalation (e.g., quiet breathing, speaking, singing, exercise, coughing, sneezing) in the form of droplets across a spectrum of sizes. These droplets carry viruses and transmit infection. The largest droplets settle out of the air rapidly, within seconds to minutes.
The way of the pathogen gets from the reservoir to the new host. For example: –
Route of transmission from respiratory tract (Nose, Mouth)
Secretion of infected person, Example: – Cough and sneezing.
Droplet transmission
Agent is coughed or sneezed out into the air
and floats on droplets.
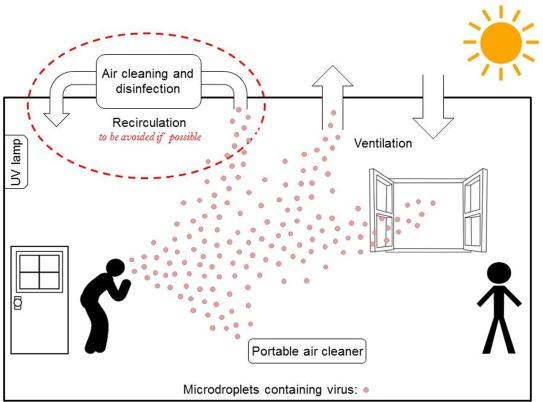
Direct spread by droplets:-
Indirect spread by droplets: –
Someone touches contaminated object.
🡪Inhalation (e.g. Respiratory tract)
🡪Ingestion (e.g. GI tract)
🡪Absorption (e.g. mucous membranes of eyes)
🡪Break in skin (e.g. Needle stick, Cut).
🡪Interaction by medical procedure (catheter).
5. The Portal of Entry
Infectious agents get into the body through various portals of entry, including the mucous membranes, non-intact skin, and the respiratory, gastrointestinal, and genitourinary tracts. Pathogens often enter the body of the host through the same route they exited the reservoir, e.g., airborne pathogens from one person’s sneeze can enter through the nose of another person.
The route through which the pathogen enters its new host
The Susceptible host
The final link in the chain of infection is a susceptible host, someone at risk of infection. Infection does not occur automatically when the pathogen enters the body of a person whose immune system is functioning normally. When a virulent pathogen enters an immune-compromised person, however, infection generally follows
A person who can get sick when exposed to a disease-causing pathogen.
How to break the chain of infection?
Ways that infection may occur.
Three things are necessary for an infection to occur: Source: Places where infectious agents (germs) live (e.g., sinks, surfaces, human skin) Susceptible Person with a way for germs to enter the body. Transmission: Way germs are moved to the susceptible person.
Factors that increase the risk of infection: –
(Hand washing).
EXAMPLE OF HOW INFECTION OCCURS
Role of health care personnel in infection control
Introduction to patient safety
Health care associated infection (HAI)
According to who:
An infection acquired in hospital by a patient who admitted for a reason other than that infection.
An infection occurs in a patient in a hospital or other health care facility in whom the infection was not present or incubating at the time of admission.
Impacts of Nosocomial infection (HIA)
Prevent from infections
Requires health care provider who have to,
– Knowledge of common infections and their vectors.
– An attitude of cooperation and commitment.
– Skills necessary to provide safe care.
-use universal precautions.
– Knowledge about the extent of the problem.
– Knowledge of main causes, modes of transmission and types of infection.
Universal precautions
Definition: universal precautions are a set of precautions designed to prevent transmission of HBV, HCV, HIV and other blood –borne pathogens while providing healthcare to all patients regardless of their diagnosis or presumed infection status.
Standard precautions:
Are the precautions to be used by all health care workers in all situations involving the care of patient of contact with the environment.
Nursing student needs